Neurology:Vogt-小柳原田病伴双侧视网膜脱离
2019-08-14 zyx整理 神经科病例撷英拾粹
28岁东非男性,表现为进行性视觉缺损和角膜炎,出现新的症状,包括头痛,恶心,平衡不能,耳鸣和右腿感觉异常。
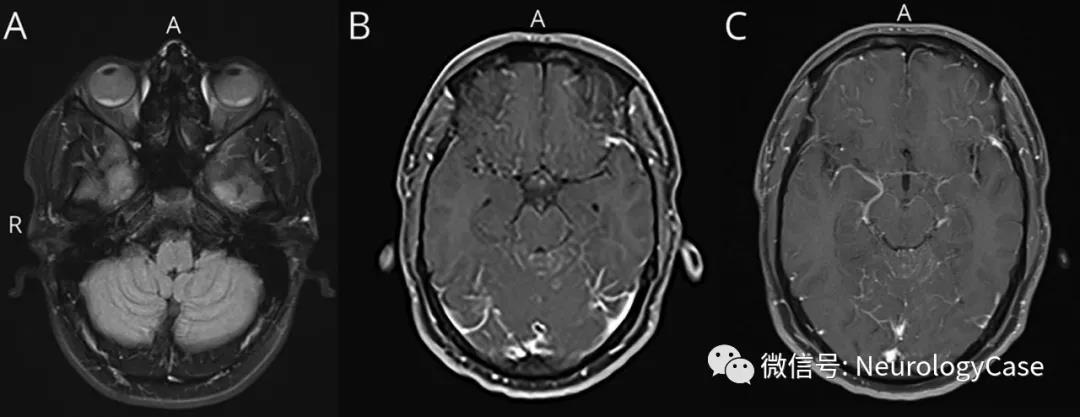
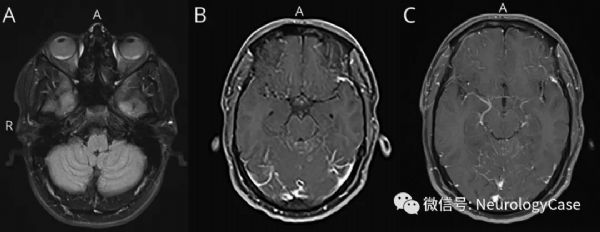
28岁东非男性,表现为进行性视觉缺损和角膜炎,出现新的症状,包括头痛,恶心,平衡不能,耳鸣和右腿感觉异常。MRI提示双侧视网膜脱离和弥漫性软脑膜强化(图)。腰椎穿刺可见淋巴细胞增多和蛋白升高。患者临床表现符合Vogt-小柳原田(VKH)病:一种自身免疫性炎症性疾病,伴眼部,听力,皮肤和神经系统受累。VKH病在亚洲,中东和西班牙裔人群中更为常见。治疗包括早期大剂量皮质类固醇激素,逐渐减量,持续数月。本例患者在大剂量甲强龙使用后症状改善。
(图:A:FLAIR可见双侧浆液性视网膜脱离和双侧视网膜/脉络膜增厚;B-C:T1增强可见软脑膜强化,以沿额叶下部和小脑内侧上部最明显)
原始出处:Al Banna M1, Reeder S2, Ghannam M2, et al. Teaching NeuroImages: A case of Vogt-Koyanagi-Harada disease with bilateralretinal detachment. Neurology. 2019 Jul 23
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Neurol#
62
#视网膜#
76
#双侧#
57