舞蹈是一种随着音乐有目的的有节奏的运动的身心活动。舞蹈可以刺激几种认知功能的神经可塑性,如学习和记忆以学习新的运动模式,注意力以遵循指令,执行功能以执行复杂的运动模式,以及社会认知以在社会互动中把运动与意义和情感表达联系起来。
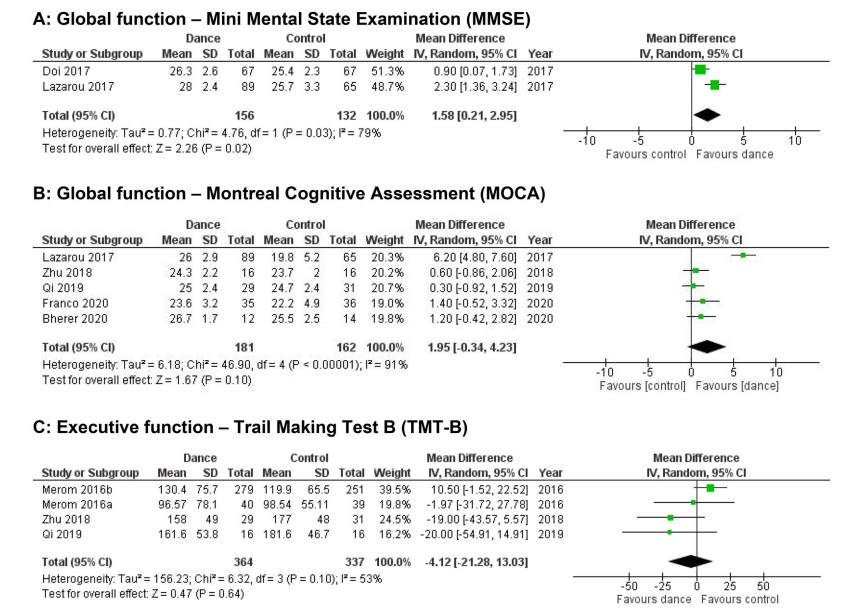
最近的证据表明,大脑结构发生了有益的变化,如海马体容积增加,灰质和白质完整。舞蹈也加强了两个大脑半球之间的连接,运动、体感和认知脑区的神经激活。为了明确舞蹈对老年人的认知功能的影响,近期发表的文章给出了答案。
来自加拿大的研究人员对MEDLINE、EMBASE、CENTRAL和PsycInfo数据库进行了搜索,时间从开始到2020年8月。纳入标准为:(i)随机对照试验;(ii)老年人(年龄≥55岁);(iii)干预-舞蹈;(iv)结果-认知功能。认知领域用《精神障碍诊断与统计手册》DSM-5神经认知框架进行分类。在RevMan5.3中进行了Meta分析,用GradePro进行了证据的确定性分析。
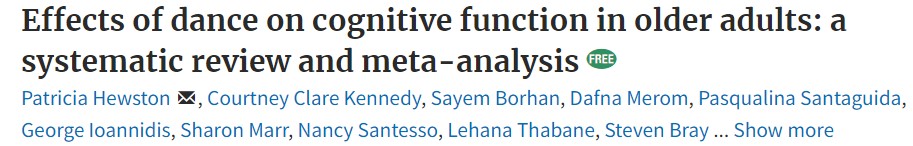
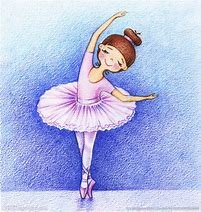
结果共回顾了3997条记录,纳入了11项研究(N = 1412名参与者)。7项研究只包括健康的老年人,4项研究包括有轻度认知障碍(MCI)的老年人。舞蹈干预的频率(1-3次/周)、时间(35-60分钟)、持续时间(3-12个月)和类型各不相同。结果发现在全脑认知功能的MMSE检查中,平均差异(MD)=1.58(95%CI=0.21-2.95)(中等确定性证据),学习和记忆的Wechsler记忆测试中,MD=3.02(95%CI=1.38-4.65;低确定性证据)。
在复杂注意力的Trail Making Test-A中,MD=3.07(95%CI=-0.81至6.95;高确定性证据),在执行功能的Trail Making Test-B中,MD=-4.12(95%CI=-21.28至13.03;中等确定性证据)。亚组分析并没有表明对患有MCI的老年人有持续的更大效果。
综上,舞蹈可能改善整体认知功能和执行功能。未来的研究需要确定最佳剂量,以及舞蹈是否比其他类型的体育活动和运动带来更大的认知益处。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#跳舞#
90
#荟萃#
119
#荟萃分析#
96
#学习##心血管#
106
老年患者多运动
0