Lancet Neuro:年轻人好端端运动就中风了?小心这一中青年人卒中“雷区”!
2021-04-06 MedSci原创 MedSci原创
研究结果支持对中青年颈动脉撕裂性中风患者使用维生素K拮抗剂进行口服抗凝治疗。
有新闻报道,有一位网络上的瑜伽达人拍摄教学视频,展示超高难度的“倒立俯卧撑”。拍摄完几个小时后,她开始视物模糊、四肢无力、头痛。两天后症状不仅没有缓解,还发现自己两个瞳孔竟然变得大小不一,这才去医院。检查结果出来,如五雷轰顶——中风。
颈动脉撕裂是<50岁中青年人中风的主要原因。根据研究报道,颈动脉撕裂导致的脑缺血事件只占所有人群缺血性卒中(俗称中风)的2%,但在中青年缺血性卒中的占比却高达10%-25%,是导致中青年缺血性卒中的重要原因。

从历史上看,临床医生更倾向于对颈动脉撕裂患者使用维生素K拮抗剂进行口服抗凝治疗。然而目前一些基于现有证据的指南通过观察性研究,建议使用阿司匹林进行治疗。如果被证明非劣于维生素K拮抗剂,阿司匹林可能可作为优选,因为它易于使用和成本较低。
那么,与维生素K拮抗剂相比,阿司匹林在颈动脉撕裂患者中的作用能否有效呢?为此,来自瑞士巴塞尔大学神经病学专家开展了相应的非劣效性研究,结果发表在最新的《柳叶刀》子刊Lancet Neurology杂志上。
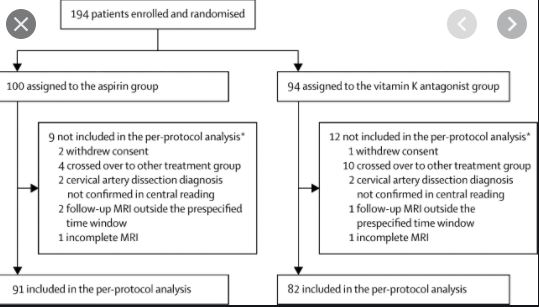
研究人员在瑞士、德国和丹麦的10个卒中中心做了一项多中心、随机、开放标签、非劣效性试验。纳入年龄>18岁、入组前2周内有症状、经MRI证实的颈动脉撕裂的患者,随机分配(1:1)接受阿司匹林300mg每日一次或维生素K拮抗剂(目标国际正常化比值[INR]维持在2.0-3.0)治疗90天。
主要终点是在开始治疗后14天(临床和MRI结果)和90天(仅临床结果)评估每个方案人群的临床结果(卒中、大出血或死亡)和MRI结果(新的缺血性或出血性脑病变)。
在2013年9月11日至2018年12月21日期间,共纳入了194名患者;100名(52%)被分配到阿司匹林组,94名(48%)被分配到维生素K拮抗剂组。阿司匹林组有21例患者(23%)和维生素K拮抗剂组的12例(15%)达到主要治疗重点(绝对差异8%,非劣效性p=0.55)。
由此可见,该研究结果未显示出阿司匹林的非劣效性。同时,阿司匹林组有7名患者(8%),维生素K拮抗剂组无一患者发生缺血性卒中。两组各有1名患者发生重大颅内出血,但都无死亡病例。阿司匹林组有14名患者(15%)和维生素K拮抗剂组有11名患者(13%)出现亚临床MRI结果。阿司匹林组有19例不良事件,维生素K拮抗剂组有26例。

综上,研究结果支持对中青年颈动脉撕裂性中风患者使用维生素K拮抗剂进行口服抗凝治疗。
参考文献:
Aspirin versus anticoagulation in cervical artery dissection (TREAT-CAD): an open-label, randomised, non-inferiority trial. https://doi.org/10.1016/S1474-4422(21)00044-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
56
学习了
76
学习了
88
#青年人#
79
#中青年#
70
非常好
163
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
107
顶刊就是不一样,质量很高,内容精彩!学到很多
113
中风是俗称,应该称为缺血性卒中吧
67
科学运动
128