Ann Med :用酪氨酸激酶抑制剂治疗的患有慢性期慢性粒细胞白血病的青少年和年轻人的结果
2022-05-02 网络 网络
AYA 患者在诊断 CML-CP 时的肿瘤负荷较高,但与接受 TKI 治疗的老年患者相比,他们的预后并不差。AYA组的MMR、EFS和OS率与老年组相当

自引入酪氨酸激酶抑制剂(TKI)治疗以来,慢性髓系白血病(CML)的预后有了显著改善。很少有研究报告患有慢性期慢性粒细胞白血病 (CML-CP) 的青少年和青年 (AYA) 对酪氨酸激酶抑制剂 (TKI) 的疗效,包括第二代TKIs尼洛替尼和达沙替尼,因此,一研究团队回顾性分析了AYA患者接受TKIs治疗的CML-CP的临床特征和结局,并进一步评估了接受尼洛替尼和达沙替尼治疗的AYA患者的结局。
研究人员回顾性分析了 42 名 AYA 患者与老年患者的临床特征、治疗反应和长期结果。2001 年-2016 年间 AYA 患者的初始治疗包括伊马替尼(n = 24)、达沙替尼(n = 13)和尼罗替尼(n = 5)。
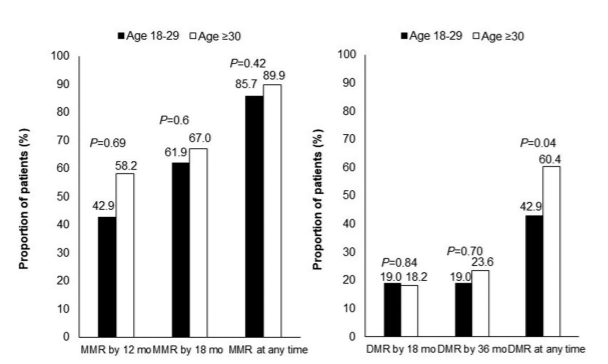
图1:根据年龄组别对TKIs的分子反应。p:AYA与老年组之间的显著性水平。MMR:主要分子反应;DMR:深度分子响应;TKI:酪氨酸激酶抑制剂。

图2:根据年龄组别对TKI的反应。(A) MMR累积发生率。(B) DMR累积发生率。p表示AYA与老年组之间的显著性水平。MMR:主要分子反应;DMR:深度分子响应;TKI:酪氨酸激酶抑制剂
在AYA患者中,诊断时外周血(PB)白细胞计数和原始细胞百分比显着升高,血红蛋白水平较低,脾脏较大。主要分子反应 (MMR)、无事件生存 (EFS) 和总生存 (OS) 率具有可比性。一项将伊马替尼与第二代 TKI 作为初始治疗进行比较的子分析也表明,它们的预后具有可比性。
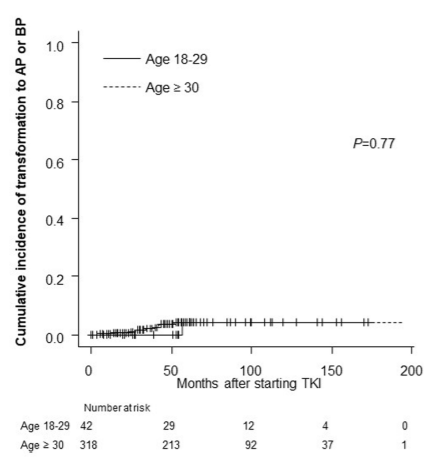
图3:不同年龄组转化为AP或BP的累积发生率
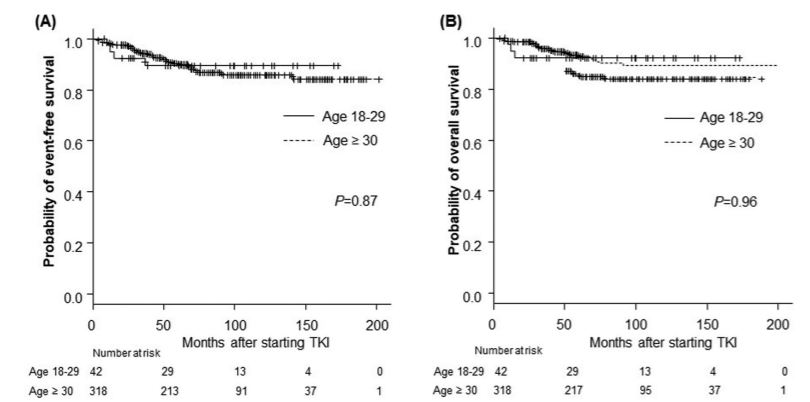
图4:根据年龄组别,TKIs治疗患者的长期结果。(A) AYA组的5年无事件生存率(EFS)为89.3%;老年组:89.8% (p .87)。(B) AYA组的5年总生存率(OS): 92.3%;老年组:92.8% (p .96)
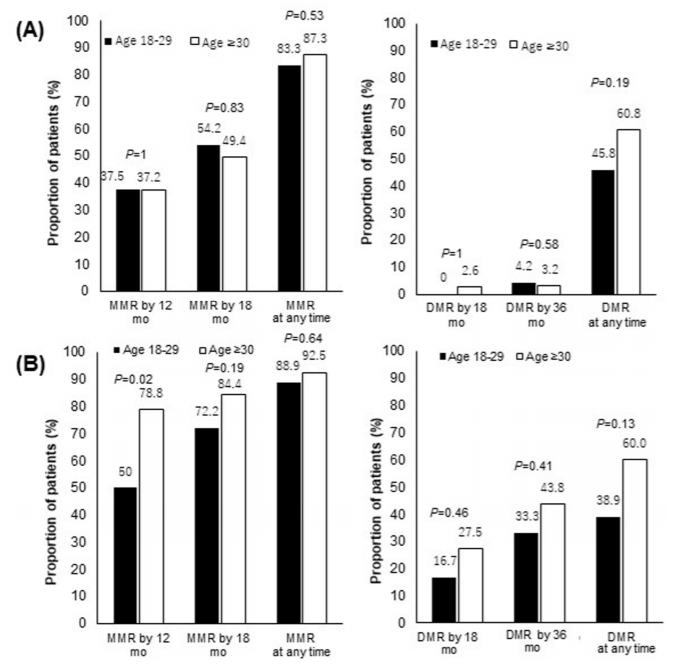
图5:根据年龄分组,对每个TKI的分子反应。(A)伊马替尼作为初始治疗的患者中根据年龄组的分子反应(N¼182)。(B)以尼洛替尼或达沙替尼作为初始治疗的患者中根据年龄分组的分子反应(N¼178)
总之,AYA 患者在诊断 CML-CP 时的肿瘤负荷较高,但与接受 TKI 治疗的老年患者相比,他们的预后并不差。AYA组的MMR、EFS和OS率与老年组相当。了解AYA CML-CP患者接受TKI治疗的生物学和非生物学特征对更好的治疗至关重要,并可能最终改善预后。
原始出处:
Nishiyama-Fujita Y, Nakazato T, Iriyama N, Tokuhira M, Ishikawa M, Sato E, Takaku T, Sugimoto K, Fujita H, Fujioka I, Tsuchiya S, Kimura Y, Iwanaga E, Komatsu N, Asou N, Kizaki M, Hatta Y, Kawaguchi T. Outcomes of adolescents and young adults with chronic-phase chronic myeloid leukaemia treated with tyrosine kinase inhibitors. Ann Med. 2022 Dec;54(1):1244-1254. doi: 10.1080/07853890.2022.2069280. PMID: 35486442.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#酪氨酸激酶#
102
#激酶抑制剂#
174
#抑制剂#
91
学习了
95
#激酶#
112
#Med#
90