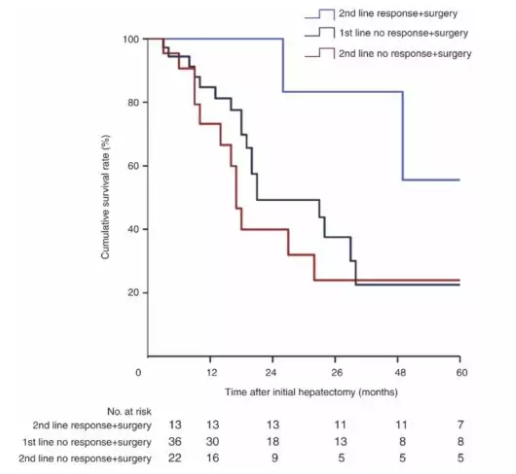
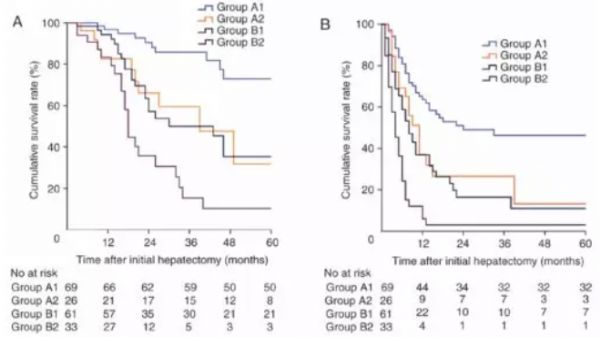
Oncology Letters:不同复发风险肝转移患者的化疗反应与手术切除的预后
2018-01-23 徐达 北京大学肿瘤医院肝胆外一
手术切除是结直肠癌肝转移(CRLM)患者获得长期生存的主要手段,但手术切除后约70%的患者会发生复发。新辅助化疗是降低复发,延长无复发生存的重要手段。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TTE#
80
#ERS#
79
#Oncol#
0
#Oncology#
76
#复发风险#
62
#化疗反应#
93
#肝转移#
69
#手术切除#
113
henhao
87
henhao
128