跟骨外侧壁完整的SandersⅢAB型跟骨骨折1例
2019-02-11 岳振双 汤样华 郑文杰 临床骨科杂志
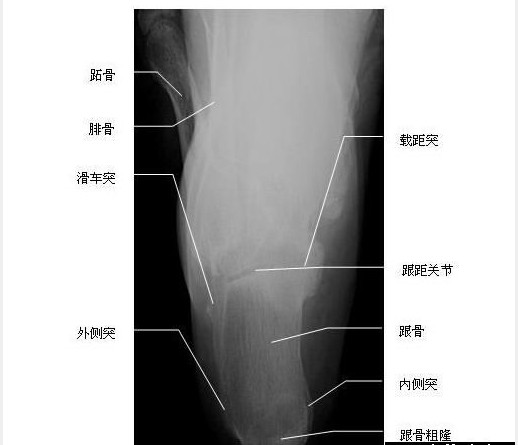
患者,男,45岁,从约1m高处坠落致右足跟肿痛畸形、行走受限2h,以右跟骨骨折急诊入院治疗。查体:右足跟及踝部肿胀明显,皮纹消失,未见张力性水疱,后足内侧皮下瘀斑,压痛阳性,足底叩击痛阳性,未触及明显骨擦感,踝关节主动背伸及跖屈活动受限。X线片显示(见图1A):右跟骨后关节面区骨小梁排列紊乱,密度增高。CT显示(见图1B~D):右跟骨后关节面中央部分塌陷压缩,跟骨外侧壁完整。明确诊断为右跟骨骨折,
临床资料
患者,男,45岁,从约1m高处坠落致右足跟肿痛畸形、行走受限2h,以右跟骨骨折急诊入院治疗。查体:右足跟及踝部肿胀明显,皮纹消失,未见张力性水疱,后足内侧皮下瘀斑,压痛阳性,足底叩击痛阳性,未触及明显骨擦感,踝关节主动背伸及跖屈活动受限。X线片显示(见图1A):右跟骨后关节面区骨小梁排列紊乱,密度增高。CT显示(见图1B~D):右跟骨后关节面中央部分塌陷压缩,跟骨外侧壁完整。明确诊断为右跟骨骨折,SandersⅢAB型。伤后第9天在硬膜外麻醉下行右跟骨骨折开放复位锁定钢板内固定术。患者左侧卧位,患肢驱血并使用气囊止血带(50kPa),取右足跟外侧扩大L形切口,显露跟距关节面,见跟骨外侧壁完整。

讨论
根据术前CT显示,使用骨刀行跟骨外侧壁V形截骨开窗,见跟骨后关节面碎裂成3部分、关节面塌陷,以内侧跟骨载距突为参照将中央塌陷的关节面顶推复位,再将跟骨后关节面外侧壁复位,克氏针临时固定,使用跟骨锁定钢板固定。术中透视确定骨折复位固定满意后逐层缝合伤口。术后采用抬高位短腿石膏固定踝关节于中立位。术后2dX线片显示骨折复位良好(见图1E)。术后4周拆除石膏,指导患者进行踝关节和距下关节的主被动功能锻炼;8周后开始指导患者进行渐进性负重功能锻炼。术后4个月患者恢复正常的生活和工作。
原始出处:
岳振双,汤样华,郑文杰等.跟骨外侧壁完整的Sanders ⅢAB型跟骨骨折1例[J].临床骨科杂志,2018,21(6):650.DOI:10.3969/j.issn.1008-0287.2018.06.003.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ERS#
119
#跟骨#
114
学习
154