JNER:多发性硬化症、帕金森病患者和健康对照者的实验室步态特征与日常生活步态特征
2021-09-11 MedSci原创 MedSci原创
步态障碍疾病在神经系统疾病患者中非常常见,导致患者跌倒风险升高和生活质量降低。步态评估助于测试新干预措施的有效性。然尽管实验室步态评估提供了实验室条件下的步态信息,但它们可能无法反映日常活动中实际的功
步态障碍疾病在神经系统疾病患者中非常常见,导致患者跌倒风险升高和生活质量降低。步态评估助于测试新干预措施的有效性。然而尽管实验室步态评估提供了实验室条件下的步态信息,但它们可能无法反映日常活动中实际的功能性步态表现。实验室中的步态评估反映了一个人的能力(一个人能做什么),而日常生活中的步态反映了一个人的功能表现(一个人实际在做什么)。因此,与日常生活功能相关的潜在步态损对于临床康复研究非常重要。
特定类型的步态障碍因神经系统疾病而异。例如,MS患者的步态特征是耐力下降、痉挛和共济失调,而PD患者的步态特征是运动迟缓、步履蹒跚、僵硬、僵硬和转动困难。步速减慢在任何神经系统疾病或年龄中都很常见。可穿戴技术的使用使得在实验室和日常生活中量化步态成为可能。将实验室中长距离稳态步态的步幅与日常生活中测量的所有步幅进行比较,会因步态长度的差异而混淆。因此,在本研究中,将重点放在实验室的短步行测试上,并将实验室中的步态特征与日常生活中类似的短步行运动进行比较。
在这项研究中,旨在确定一组步态测量方法,该方法能够从实验室的单个短步行步态测试中最好地区分MS患者与健康对照受试者,以及PD患者与健康对照受试者之间的步态特征,并使用可穿戴传感器将这些步态质量测量值与一周的日常生活步态质量测量值进行了比较。本文发表在《Journal of NeuroEngineering and Rehabilitation》。

招募了MS组、PD组年轻,以及与其年龄对应的年轻和老年对照组进行比较。具体而言,帕金森病的纳入标准是运动障碍神经学家根据英国帕金森病学会脑库标准诊断特发性帕金森病。MS的纳入标准为神经科专家确认的诊断标准。
受试者佩戴3个惯性传感器。每个传感器包括一个采样率为128 Hz的三轴加速计、陀螺仪和磁强计。传感器重量轻(22克),电池寿命为16小时,包括8 GB的存储空间,可记录30天以上的数据。所有受试者都进行了仪器化站立和行走测试(ISAW)。
ISAW包括安静地站立30秒,然后口头指示开始步态,步行7米,穿过地面上的一条线后转向180度,然后返回初始起始位置。ISAW测试设计用于在一个短测试中测量姿势摆动、步态开始、步态和转向。MS患者完成了MS严重程度的评估,患者完成了扩展残疾状态量表(PREDSS),多发性硬化症步行能力量表(MSWS-12),以及改良疲劳指数量表(MFIS))。PD严重程度由认证研究人员使用运动障碍学会统一帕金森病评定量表(MDS-UPDRS)第三部进行评估。所有受试者在服用常规药物(服药状态)后1小时在实验室进行测试,因为大多数情况下,受试者试图在日常生活中处于服药状态。
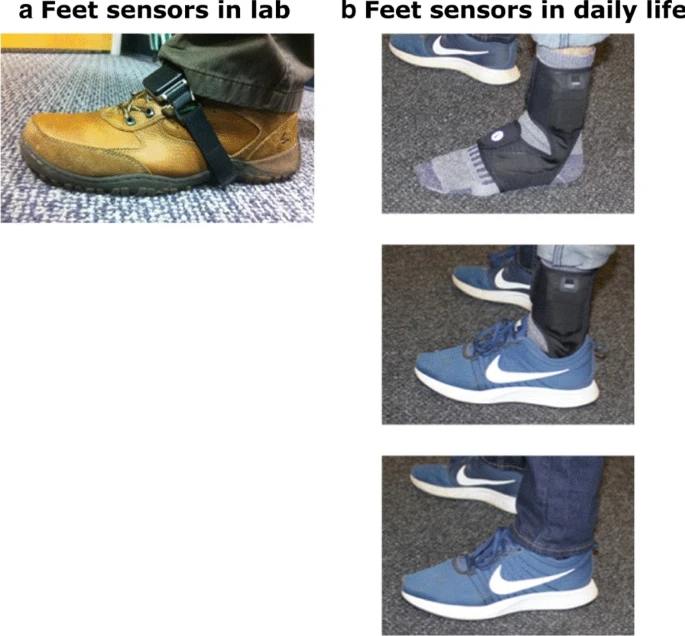
足部佩戴传感器
为了在实验室和日常生活步态测量之间进行比较,使用了在实验室ISAW测试期间和日常活动期间步幅数量相似的步态测试(大约4-15步)。具体而言,计算了所有参与者在实验室进行ISAW测试的有效步幅数,发现其范围在4到15步之间,使用了与实验室ISAW测试中观察到的步幅范围相同的范围(4到15步)。
15名MS患者、16名年龄匹配的健康人对照组、16名PD患者以及15名年龄匹配的PD健康人参与了本研究。参与者在日常生活中佩戴传感器60-68小时。在实验室步态测试和一周的日常生活中,最能区分MS和PD患者各自对照组步态特征的测量方法是不同的。具体而言,在实验室中,脚趾离地角度最能区分MS和MS健康对照组。相比之下,在实验室中,腰椎运动范围最能区分PD和PD健康对照组。
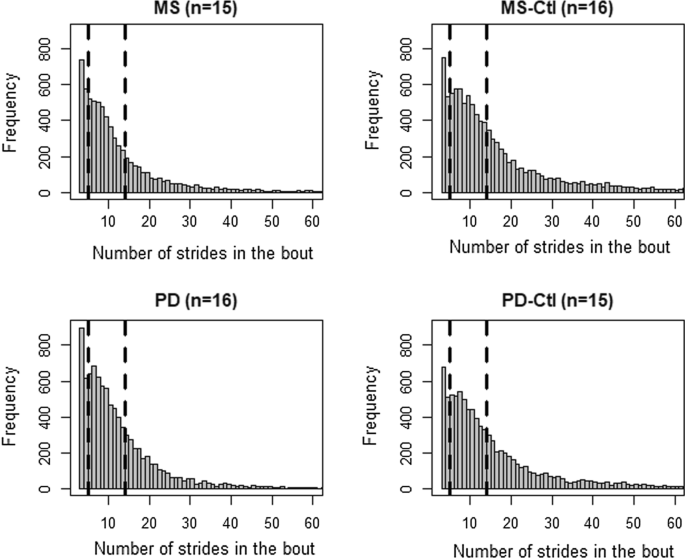
各组在日常生活中的结果直方图
在实验室和日常生活中,区分MS患者和MS对照组步态特征的方法不同 。具体而言,在实验室中,脚趾离地角度是最具辨别力的 ,而步态速度是日常生活中最具辨别力的 。步幅是实验室中第二好的鉴别指标。在实验室和日常生活中,鉴别PD患者步态特征和PD对照组步态特征的大多数方法是不同的。具体而言,在实验室中,腰椎冠状运动范围是最具辨别力的,而脚部触角是日常生活中最具辨别力的,而步态速度是日常生活中的辨别力。
总之,日常生活监测可能对神经疾病的损害更敏感,但每种神经疾病可能需要不同的步态结果测量。
Shah, V.V., McNames, J., Mancini, M. et al. Laboratory versus daily life gait characteristics in patients with multiple sclerosis, Parkinson’s disease, and matched controls. J NeuroEngineering Rehabil 17, 159 (2020). https://doi.org/10.1186/s12984-020-00781-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#对照#
97
#硬化症#
86
#多发性#
105
#步态#
92
#帕金森病患者#
102
#帕金森病患#
103
有助于患者
155