Ann Hematol :外周插入的中心静脉导管可减少与中心线相关的血流感染并改变成人血液学单元的微生物流行病学:倾向评分调整分析
2022-07-19 网络 网络
这项研究证实,PICC 是 CICC 在成人血液科预防 CLABSI 的更好替代品,同时它在当地流行病学中带来了微生物学的转变。
与中心静脉导管 (CICC) 相比,外周中心静脉导管 (PICC) 在预防中心静脉相关血流感染 (CLABSI) 方面具有潜在优势。然而,由于研究数量有限且统计评估不足,PICCs的优越性难以在成人血液学单元中推广。一研究团队进行了一项单中心回顾性研究,并通过传统的多变量模型和倾向评分调整分析比较了 472 例 CICC 和 557 例置入成年血液病患者的 PICC 之间的 CLABSI 风险。
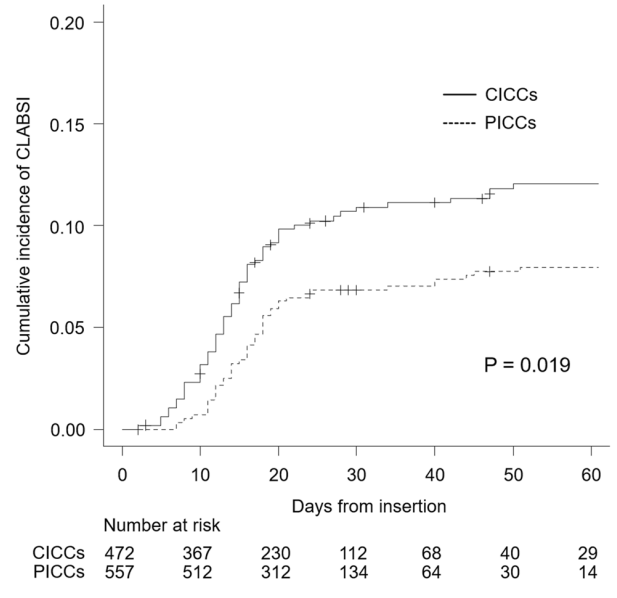
图:CICCs和PICCs中中心线相关血流感染(CLABSI)的累计发生率(连续线:CICCs;虚线:PICCs)
CICC 和 PICC 的 CLABSI 每1000个导管*天的总发病率分别为 5.11和 3.29(P = 0.024)。多变量 Cox 回归分析(风险比 [HR]:0.48;95% 置信区间 [CI]:0.31–0.75;P = 0.001)和 Fine-Gray 子分布分析(HR:0.59;95% CI:0.37–0.93;P = 0.023)表明 PICC 与 CLABSI 风险降低独立相关。
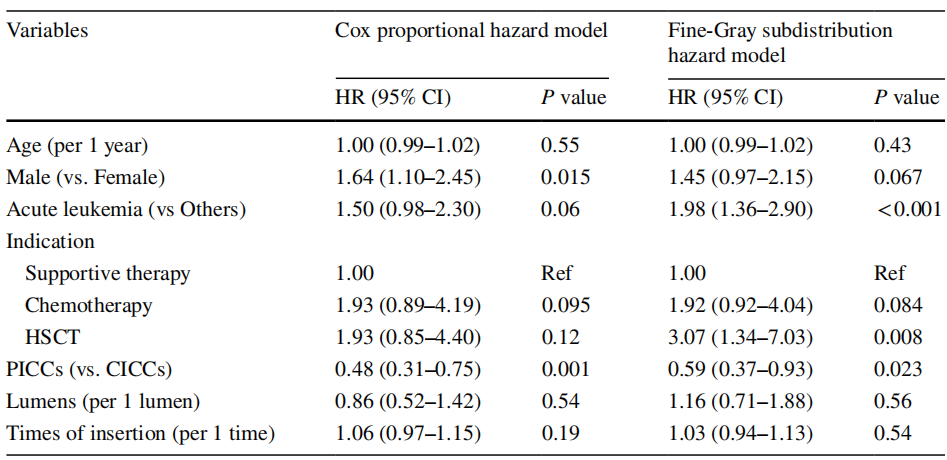
表:对CLABSI的多变量分析。CI可信间隔、CLABSI中心线相关血流感染、CICC中心插入中心静脉导管、HR风险比、HSCT造血干细胞移植、PICC外周插入中心静脉导管,参考文献
此外,稳定的治疗加权逆概率分析进一步降低了 CICC 和 PICC 之间的选择偏差,表明 PICC 显着预防 CLABSI(HR:0.58;95% CI:0.35-0.94;P = 0.029)。微生物学上,PICCs 显示革兰氏阳性球菌显着减少(P = 0.001),革兰氏阳性杆菌增加(P = 0.002),因为显着减少葡萄球菌和导致CLABSI的棒状杆菌种类增加。
总的来说,研究人员通过使用包括倾向评分调整分析在内的几种统计方法,证明了PICCs的CLABSI风险低于成人血液学单元的CICCs。PICCs对CLABSI预防的益处可能不仅是由于其更好的局部皮肤状况,而且还包括与PICC相关的维持护理。此外,PICCs在CLABSI中引起了GPC到GPB的微生物学转变,并出现了棒状杆菌在医院爆发的威胁。研究人员提出,需要进一步的研究来建立一种新的策略来解决血液病患者中CLABSI的微生物学变化。
原始出处:
Nakaya, Y., Imasaki, M., Shirano, M. et al. Peripherally inserted central venous catheters decrease central line-associated bloodstream infections and change microbiological epidemiology in adult hematology unit: a propensity score-adjusted analysis. Ann Hematol (2022). https://doi.org/10.1007/s00277-022-04908-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#微生物#
129
#静脉#
94
#中心静脉#
106
#EMA#
145
#中心静脉导管#
0
#流行病#
101
#血液学#
95
#血流感染#
102