Blood:弥漫性大B细胞淋巴瘤CD37基因免疫优势位点的高发突变
2019-08-02 MedSci MedSci原创
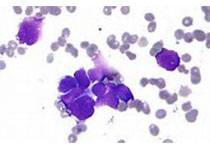
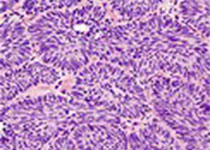
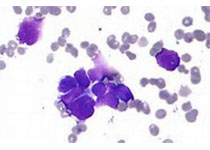
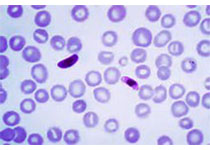
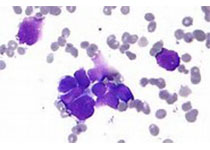
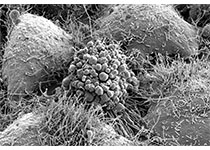
四次跨膜蛋白CD37主要表达于成熟B淋巴细胞表面,目前正被作为治疗B细胞淋巴瘤的新靶点进行研究。近期,研究人员发现在Cd37敲除的小鼠中,CD37缺失可诱导形成自发性B细胞淋巴瘤,而且还与弥漫性大B细胞淋巴瘤(DLBCL)患者的预后不良相关。
CD37突变型淋巴瘤B细胞表现为CD37细胞表面定位受损,这使抗CD37治疗或可以治疗B细胞淋巴瘤
摘要:
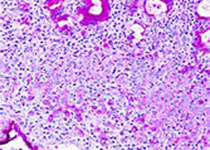
CD37突变在IP-DLBCL病例中的外显率高达23%(10/44),但在非IP-DLBCL病例中未检测到CD37突变。检测到的CD37突变包括10个错义突变、1个缺失和3个剪接位点突变。CD37错义突变的建模和功能分析显示,功能性丧失表现位淋巴瘤B细胞细胞膜上的CD37蛋白表达受损。
本研究为深入研究IP-DLBCL的分子机制提供了新的思路,提示抗CD37治疗对无CD37突变的DLBCL患者更有益。
Suraya Elfrink, et al.High frequency of inactivating tetraspanin CD37 mutations in diffuse large B-cell lymphoma at immune-privileged sites.Blood 2019 :blood.2019001185; doi: https://doi.org/10.1182/blood.2019001185
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#细胞淋巴瘤#
88 举报
#B细胞#
84 举报
#弥漫性大B细胞淋巴瘤#
96 举报
#弥漫性#
98 举报
#CD37#
100 举报
学习了
122 举报
不错
122 举报