Alzheimer Dementia : 肿瘤坏死因子抑制剂,或可降低痴呆风险
2021-10-05 Freeman MedSci原创
在患有RA的美国退伍军人中,使用TNF抑制剂与降低痴呆/AD的长期风险有关。
随着世界人口的老龄化,痴呆症是一个全球性的健康问题。阿尔茨海默病(AD)是最常见的痴呆形式,占50%至80%的病例;其他形式的痴呆包括血管性、路易体和额颞性。越来越多的证据表明,脑血管炎症在痴呆症中起着重要的作用,特别是在与AD患者大脑中淀粉样β和tau积累有关的病理过程中。由小胶质细胞和其他免疫细胞过度激活介导的持续炎症反应,已被证明会加剧淀粉样蛋白和tau的病理变化。肿瘤坏死因子(TNF)是启动和控制炎症过程的关键促炎细胞因子。多种证据表明,TNF可能触发或放大大脑中异常的小胶质细胞信号,从而促进AD发病机制。
类风湿性关节炎(RA)是一种常见的自身免疫性系统性炎症疾病,影响到全球约1%的人口。根据最近的一项研究,RA患者中痴呆症的总发病率为0.79%。RA可能是研究炎症在痴呆症发展中的作用的一个很好的模型,因为TNF在这两种情况下都发挥着重要作用,而且TNF抑制剂药物是治疗RA的有效方法。因此,研究抗TNF治疗对RA患者痴呆风险的影响可能为重新利用TNF抑制剂治疗痴呆和AD提供机会。
多年来,炎症途径一直是痴呆/AD治疗的目标。许多关于非甾体抗炎药(NSAIDs)的流行病学研究报告,NSAIDs与痴呆/AD风险的降低有关。然而,这些研究大多样本量较小,最终,大多数基于NSAIDs的随机试验未能显示出对痴呆/AD患者的益处。目前,传统的改变病情的抗风湿药物(cDMARDs)被用作治疗RA的一线药物。有两项研究报告了cDMARDs与痴呆/AD风险的关系,但结果相反。最近的一项临床试验考察了羟氯喹对早期AD患者痴呆症进展的影响,结果显示没有有益的影响。20 一些观察性研究已经进行了研究,调查了RA患者使用TNF抑制剂与痴呆症的关系。一项使用台湾国家健康保险研究数据库2000年至2011年数据的回顾性病例对照研究显示,使用TNF抑制剂与痴呆症发病率之间没有明显的关联(几率[OR]:0.71,95%置信区间[CI]:0.46-1.10,957名匹配患者)。
一项使用2000年至2007年健康保险索赔数据的嵌套病例对照研究显示,TNF抑制剂作为一类药物与较低的AD风险有关(调整OR 0.45;95%CI 0.23-0.90,165名合格的AD患者)。对于单个TNF抑制剂,只有依那西普显示AD风险降低(调整后OR为0.30;95%CI为0.08-0.89)。然而,这两项研究的样本量有限。
最近的研究使用了一个全国性的电子健康记录(EHR)数据库,包括514,440名RA患者,也显示TNF抑制剂的使用和较低的AD风险有明显的关联。所有以前的研究都有有限的研究期(7年和11年),而且病人的实际随访时间也不清楚,所以使用TNF抑制剂对痴呆和AD风险的长期影响仍然是未知的。
藉此,美国CaseWestern Reserve University的Chunlei Zheng 使用2000年至2020年全国范围内的退伍军人健康管理数据库(VHA)的EHR来调查RA患者使用TNF抑制剂与痴呆症风险的关系。
退伍军人管理数据库是美国最大的综合医疗保健系统,每年为900多万病人提供护理。VHA服务的患者群体在临床试验中的代表性经常不足,尤其是大部分的老年患者。
此外,VHA运营着一个EHR系统,无论VHA的护理地点在哪里,记录都会被汇总到一个集中的数据库中,这使得在一个流动的真实世界中进行更长时间的跟踪研究成为可能。大样本量、集中于老年患者和长时间的随访使VHA的EHR数据成为研究TNF抑制剂对痴呆和AD风险影响的独特资源。在这项回顾性队列研究中,他们评估了TNF抑制剂与RA患者痴呆风险的关系,随访时间长达20年。
他们从2000年到2020年,在美国退伍军人事务保健系统内的40207名RA患者中进行了倾向性评分匹配的回顾性队列研究。
他们发现:共有2510名RA患者使用TNF抑制剂,与对照组患者1:2匹配。
使用TNF抑制剂与痴呆风险的降低有关(危险比[HR]:0.64,95%置信区间[CI]:0.52-0.80).
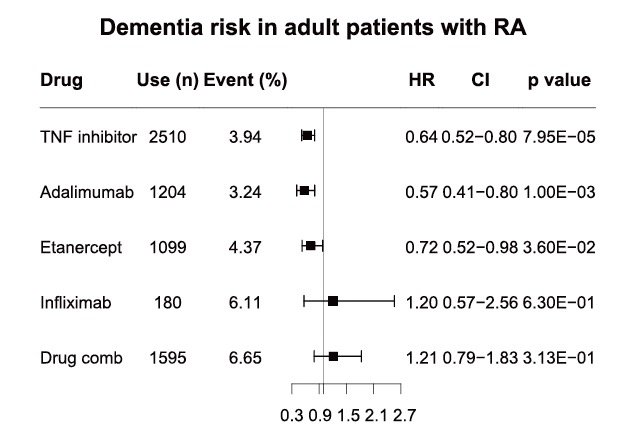
随着研究期从RA诊断后5年到20年的增加,这种情况是一致的。在20年的随访中,使用TNF抑制剂也显示出降低AD风险的长期效果(HR:0.57,95% CI:0.39-0.83)。
这个研究的重要意义在于发现了:在患有RA的美国退伍军人中,使用TNF抑制剂与降低痴呆/AD的长期风险有关。
原文出处:
Zheng C, Fillmore NR, Ramos‐Cejudo J, et al. Potential long‐term effect of tumor necrosis factor inhibitors on dementia risk: A propensity score matched retrospective cohort study in US veterans. Alzheimer’s & Dementia. Published online September 27, 2021:alz.12465. doi:10.1002/alz.12465
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#抑制剂#
84
#dementia#
73
学习
97
#肿瘤坏死因子抑制剂#
118
#痴呆风险#
79
#坏死#
117
#肿瘤坏死因子#
149
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
96