Alzheimer Dementia:认知和步态功能越弱,痴呆风险越高
2021-12-08 Freeman MedSci原创
MCR可能代表了一种痴呆症前综合征,其特征是突出的白质异常和额叶萎缩。
运动性认知风险(MCR)的特点是主观认知障碍和缓慢步态的共同出现,与认知障碍和随后的痴呆(也称为主要神经认知障碍)的风险增加有关。单独的缓慢步态与痴呆的风险增加有关,特别是血管性和其他非阿尔茨海默病(AD)痴呆。
同样,以步态速度和记忆力同时下降为特征的表型(双重下降者)也与痴呆风险和脑容量损失有关。步态缓慢和认知能力下降的共同出现--在双重下降者的情况下是客观的,在MCR的情况下是主观的--似乎比任何一个因素单独出现更能预示痴呆症的准确性。
虽然MCR可能与其他痴呆症前期综合征重叠,特别是轻度认知障碍(MCI),但MCR和MCI可以而且经常独立发生。MCR作为痴呆症前期综合征的预测能力已经确定,但MCR的神经病理学基础,以及它们是否与MCI不同,仍然是未知的。
研究将MCR与额叶隙性梗死和额叶灰质体积减少联系起来,支持MCR可能代表额叶-皮层下脑血管疾病的临床表现的观点。然而,使用神经影像学检查MCR的神经病理学特征的研究很少,依赖于适度的样本量,并且没有纳入AD分子生物标志物,如淀粉样蛋白。
藉此,约翰霍普金斯大学的Gabriela T. Gomez等人,利用社区动脉粥样硬化风险研究(ARIC)的一个大型社区样本,旨在探究:(1)复制MCR与发生痴呆的关联,(2)研究MCR是否与大脑结构和分子异常的特定模式有关,以及(3)间接比较MCR与MCI的神经影像学特征。
他们基于社区的动脉粥样硬化风险(ARIC)社区队列研究在研究基线(2011-2013年)使用标准化标准将参与者分为MCR+/-和轻度认知障碍(MCI)+/-。并研究了与MCR+和MCI+状态相关的5年痴呆风险和基线大脑结构/分子异常。
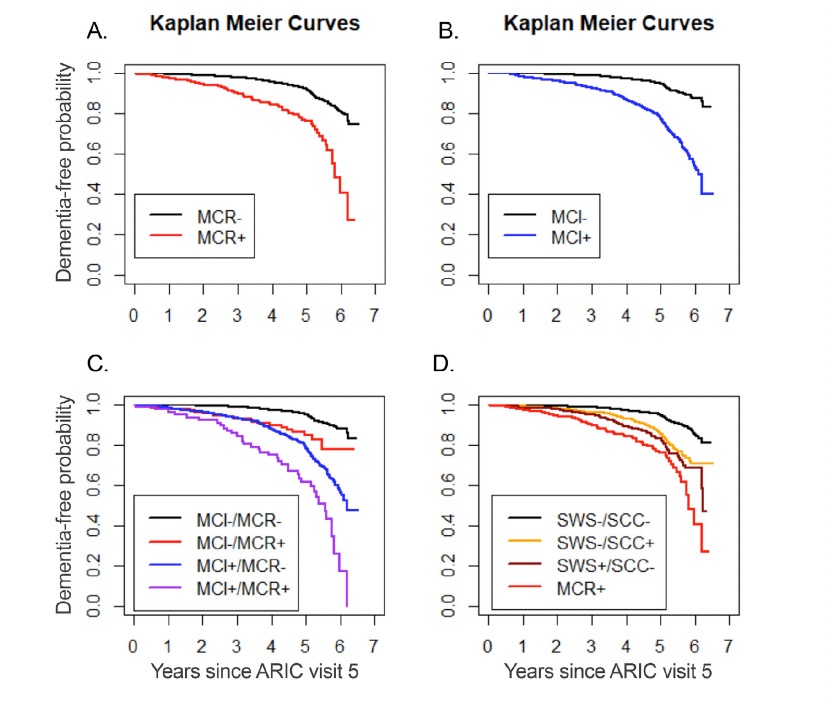
在纳入的5023名非痴呆参与者中,204人是MCR+,1030人是MCI+。MCR+和MCI+参与者都显示出痴呆风险增加。
与MCR+相关的大脑结构异常的模式与MCI+不同。
MCI+与易患阿尔茨海默病的脑区体积相对较小有关,而MCR+状态与额叶区的体积较小和白质异常较大有关。
这个研究的重要意义在于发现了: MCR可能代表了一种痴呆症前综合征,其特征是突出的白质异常和额叶萎缩。
原文出处:
Gomez GT, Gottesman RF, Gabriel KP, et al. The association of motoric cognitive risk with incident dementia and neuroimaging characteristics: The Atherosclerosis Risk in Communities Study. Alzheimer’s & Dementia. Published online November 17, 2021:alz.12412. doi:10.1002/alz.12412
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#dementia#
90
#步态#
118
#痴呆风险#
92
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
86