Movement disorders 同济大学;帕金森病:短链脂肪酸减少,或因肠-血屏障受损
2022-06-29 Freeman MedSci原创
PD患者的粪便和血浆SCFAs的改变与GBB受损有关,并可能因便秘而加重。
帕金森病(PD)是一种神经退行性疾病,以运动症状为特征,包括运动迟缓、静止性震颤和僵硬。其病理特征是α-synuclein在大脑中的异常聚集。PD患者还经常表现出非运动症状(NMS),包括胃肠道功能障碍,尤其是早期出现的便秘。
 图1: 论文封面图
图1: 论文封面图
此外,肠道α-synuclein的积累在运动症状出现之前就已经被检测出来。目前的假说认为,PD的病理生理过程可能源于肠道神经系统。PD患者的肠道微生物群与健康人明显不同,并被认为通过肠道-大脑轴在PD的发生和发展中发挥了重要作用。
细菌膳食纤维在肠道内发酵产生的短链脂肪酸(SCFAs)在维持肠道屏障和增加胃肠道蠕动方面起着重要作用。据报道,PD患者的粪便乙酸(AA)、丙酸(PPA)和丁酸(BA)明显减少,而另一项研究显示PD患者的血浆AA浓度更高。这些研究没有发现PD患者的粪便和血浆中SCFAs的同步变化,同时还有肠道-血液屏障(GBB)的渗透性指标。
因此,粪便和血浆中的对比变化的整体方案和原因仍然未知。大约40%-80%的PD患者表现出便秘或结肠转运时间延长,这对PD相关的微生物群组成有深刻的影响。此外,结肠转运时间的延迟导致微生物代谢从碳水化合物发酵转向蛋白质分解,这影响了肠道SCFAs的产生。因此,结肠转运时间对肠道微生物组成和功能的强烈影响强调了在微生物代谢物研究中考虑结肠转运时间这一混杂因素的重要性。
藉此,同济大学的Xiaodong Yang等人,描述了PD患者队列中粪便和血浆SCFAs的同步改变,并通过将便秘作为混杂因素来确定SCFAs与PD的具体关联。
他们分别用液相和气相色谱质谱法测量了33名健康对照组和95名PD患者的粪便和血浆中SCFAs的浓度。PD患者被分为无便秘的PD患者(n = 35)和有便秘的PD患者(n = 60)。通过血浆/粪便中SCFA浓度的比率和粪便中α1-抗胰蛋白酶的浓度来评估肠道-血液屏障(GBB)的渗透性。
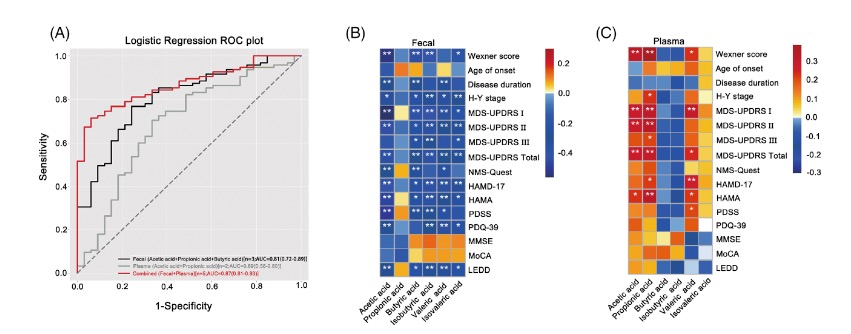 图2:论文结果图
图2:论文结果图
PD患者显示出粪便中乙酸、丙酸和丁酸的浓度下降,血浆中乙酸和丙酸的浓度上升。
与无便秘的PD患者相比,有便秘的PD患者的粪便乙酸、异丁烯酸和异戊烯酸的浓度更低,血浆乙酸和丙酸的浓度更高。便秘加剧了PD患者的GBB渗透性。
粪便和血浆中的SCFAs可以区分PD患者和健康对照对象。
除丙酸外,粪便SCFAs与疾病严重程度呈负相关,而血浆乙酸、丙酸和戊酸呈正相关。
该研究的重要意义在于发现了:PD患者的粪便和血浆SCFAs的改变与GBB受损有关,并可能因便秘而加重。
原文出处:
Yang X, Ai P, He X, et al. Parkinson’s Disease Is Associated with Impaired Gut–Blood Barrier for Short‐Chain Fatty Acids. _Movement Disorders_. Published online May 24, 2022:mds.29063. doi:[10.1002/mds.29063](https://doi.org/10.1002/mds.29063).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#Dis#
161
#disorders#
100
#Disord#
104
#disorder#
104
#ERS#
103
#同济大学#
109