Front Oncol:淋巴结数目检查不足对II期结肠癌患者生存的影响
2021-10-29 yd2015 MedSci原创
在II期结肠癌患者中,<8个淋巴结检查的N0期患者预后较N1期患者差。在临床实践中需要更多的重视。原始出处:
结肠癌是全球最常见的恶性肿瘤之一。美国癌症联合委员会(AJCC)提出的肿瘤淋巴结转移(TNM)肿瘤分期系统已被广泛用于指导结肠癌患者的治疗方案和评估预后。根据这个分期系统,II期和III期结肠癌最明显的区别是存在病理性淋巴结转移。由美国病理学家协会(ACP)和美国癌症联合委员会(AJCC)推荐,手术标本中淋巴结的检查应至少为12个,这已成为结肠癌患者准确淋巴结分期的普遍共识。尽管如此,检查淋巴结数不足的情况并不少见。检查的淋巴结数量不足可能会导致对淋巴结受累情况的不准确评估,从而误导临床治疗决策,对患者的预后产生不利影响。一项大型回顾性研究报告发现,淋巴结检查的数量介于5.5和21.3之间淋巴结,淋巴结切除平均为11.7个,低于推荐的最小淋巴结检查数。因此,复旦大学附属中山医院的团队开展了研究,目的是评估在II期结肠癌中检查淋巴结数目不足的预后价值。相关结果发表在Frontiers in Oncology杂志上。

研究中使用的癌症数据来自SEER数据库。共筛查出80,296名II/III期结肠癌患者,收集人口统计学和临床病理特征,包括肿瘤分级、性别、诊断时间、TNM分期、种族、肿瘤组织学和接受化疗。除了II期结肠癌外,我们还招募了III期(T3期4期伴淋巴结转移)患者,以比较淋巴结检查不充分和病理淋巴结阳性的预后。男性患者占48.0%(38537例)。随访结束时共死亡45146例(56.2%)。总共有58,799名患者(73.2%)检查了12个以上的淋巴结。卡方检验结果也显示,白人(p = 0.013)、≤75岁(p<0.001)、T3期(p = 0.034)、N2期(p<0.001),差/间变性分级(p<0.001),女性(p<0.001),粘液/印戒细胞组织学(p<0.001),诊断年份较晚(p<0.001)更有可能检查足够(≥12)淋巴结。
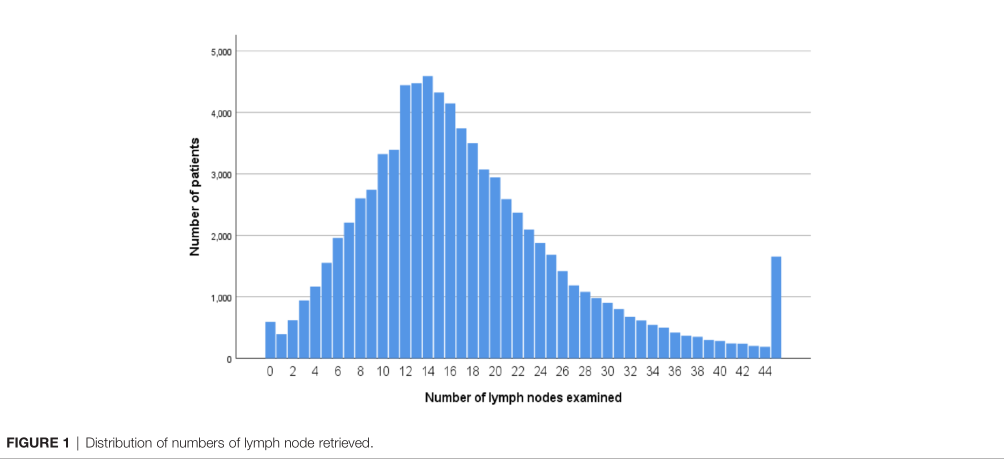
检查淋巴结数目
研究表明,淋巴结阴性患者中,随着检查淋巴结数量的减少,患者的OS更差。<4个淋巴结5年OS率= 46.2%; <8个淋巴结5年OS率= 54.1%; <12个淋巴结5年OS率= 60.2%; ≥12个淋巴结5年OS率= 69.0%。Kaplan Meier分析结果显示,与N1期相比,<8个淋巴结检查的N0患者中更有可能导致OS降低(5年OS率,54.1% vs. 57.1%, p<0.001)。此外,N1期患者的OS较<4个淋巴结检查的N0期患者有明显改善(HR = 0.909, 95%CI = 0.860 0.962, p = 0.001)。

为了更好地评估在II期结肠癌中检查淋巴结数量不足的临床作用,研究比较了淋巴结阳性患者和淋巴结阴性患者(检查淋巴结数量不足)之间的OS差异。N0期患者<8个淋巴结的OS较N1期患者的差(5年OS率, 51.6% vs. 57.1%, p < 0.001)。而<12个淋巴结检查的N0期与N1期的生存率差异无统计学意义(p = 0.918)。

多变量分析提示,< 8个淋巴结检查的N0期的OS在调整其他公认预后因素后与N1期相似(HR = 1.051, 95%CI = 1.014, 1.090, p = 0.018)。
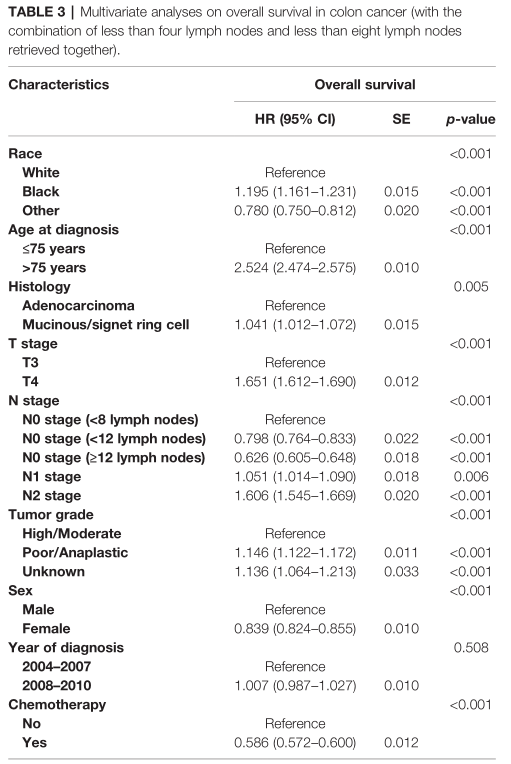
预后因素
综上,在II期结肠癌患者中,<8个淋巴结检查的N0期患者预后较N1期患者差。在临床实践中需要更多的重视。
原始出处:
Wu Q, Zhang Z, Chen Y, Chang J, Jiang Y, Zhu D and Wei Y (2021) Impact of Inadequate Number of Lymph Nodes Examined on Survival in Stage II Colon Cancer. Front. Oncol. 11:736678. doi: 10.3389/fonc.2021.736678
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Oncol#
67
谢谢分享
71
#患者生存#
75
#淋巴结#
88
谢谢分享!
87
谢谢分享
95