EMI:2009 - 2019年中国浙江地区肺炎球菌结合疫苗供应对肺炎链球菌感染和基因重组的影响
2022-02-17 从医路漫漫 MedSci原创
肺炎球菌性肺炎是全球儿童死亡的主要原因之一。肺炎球菌结合疫苗(PCV)被认为是预防肺炎球菌病(PD)最有效的方法,但暂停接种PCV疫苗如何影响PD的流行或肺炎链球菌的遗传进化尚不清楚。

背景及目的:肺炎球菌性肺炎是全球儿童死亡的主要原因之一。肺炎球菌结合疫苗(PCV)被认为是预防肺炎球菌病(PD)最有效的方法,但暂停接种PCV疫苗如何影响PD的流行或肺炎链球菌的遗传进化尚不清楚。基于中国PCV引入时间(2015年4月- 2017年4月期间疫苗无法获得),我们旨在评估中断的PCV获取对PD和肺炎球菌基因组变异的影响。
方法:回顾性收集2009年至2019年中国浙江省8个地点的肺炎球菌分离株(n=386),鉴定出184株致病性(来自无菌和感染地点的分离株)菌株。通过中断时间序列分析估计PD的变化,并通过SNP呼叫估计全基因组测序菌株的重组频率。
结果:我们发现PD和肺炎球菌基因组变异都受到PCV中断的影响。所有LRTI病例中疫苗型肺炎球菌LRTI (VT-LRTI)的比例(约70%)在PCV7晚期下降至约30%,在2015年4月PCV7失效后反弹至~70% (p=0.00 07)。PCV去除后,CC271主要克隆株重组频率从2.82±1.16降低到0.72±0.21,重组速度减慢(p=0.0293)。

表1 致病性和定殖性肺炎球菌分离株的分布。
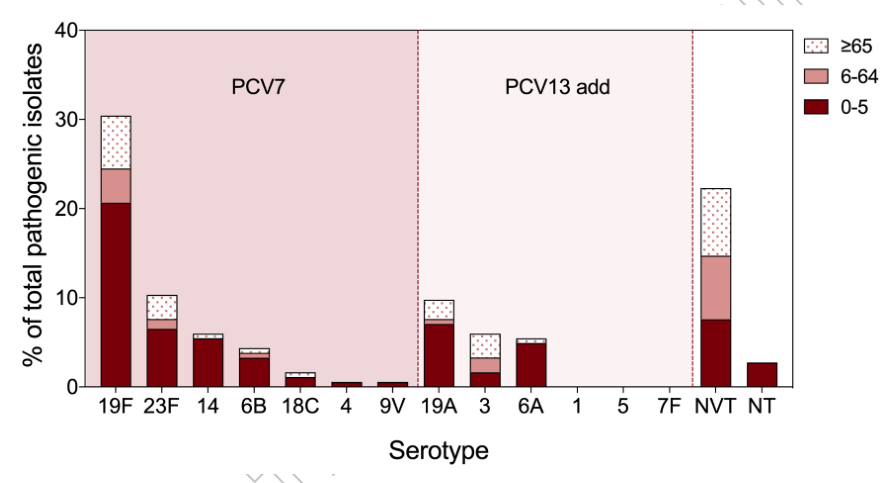
图1 致病性肺炎球菌在不同年龄组的血清型分布。
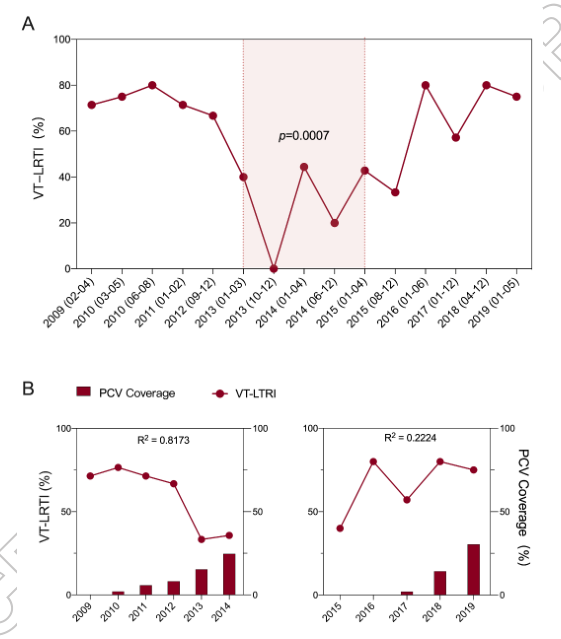
图2 疫苗型肺炎球菌相关下呼吸道感染(VT-LRTI)比例及其与PCV覆盖率的相关性
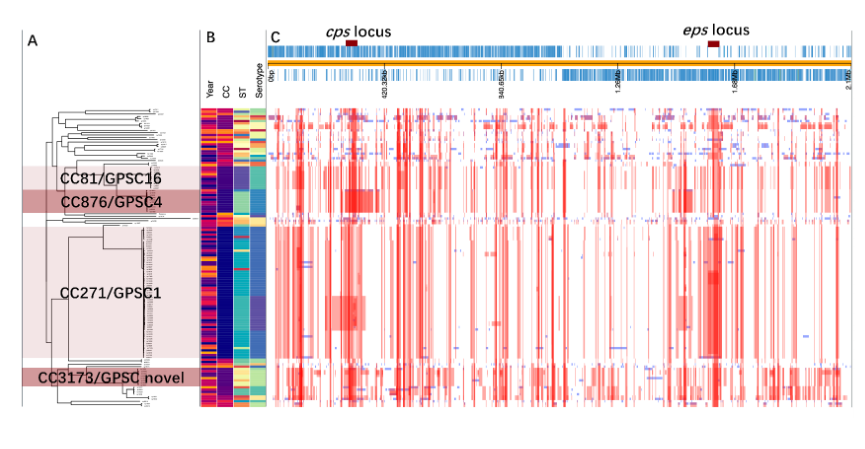
图3 5岁以下儿童肺炎球菌分离株的系统发育树和重组事件。

图4 5岁以下儿童肺炎球菌分离株的重组频率(r/m)和数量(re)。
结论:我们的研究首次表明,VT-LRTI随着中国疫苗供应中断而波动,并导致疫苗类型重组频率下降。促进全国持续的疫苗接种计划和加强肺炎链球菌分子流行病学监测对PD预防至关重要。
原文出处:Wu X, Zhao S, Jiang Y, et al.Streptococcus pneumoniaeEffect of pneumococcal conjugate vaccine availability on infections and genetic recombination in Zhejiang, China from 2009 to 2019.Emerg Microbes Infect 2022 Feb 08
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







又长知识了
103
#肺炎链球菌#
89
#肺炎球菌#
117
#链球菌#
96