Neurology:高甘油三酯血症对动脉粥样硬化性血栓性脑卒中患者预后的影响
2022-04-04 Naomi MedSci原创
颈部大动脉动脉粥样硬化性狭窄是缺血性卒中的常见原因。 高甘油三酯血症被认为促进动脉粥样硬化病理学,是一个重要的可改变的危险因素,促使动脉粥样硬化血栓性卒中患者的残余血管风险,即使在他汀治疗期间。
颈部大动脉动脉粥样硬化性狭窄是缺血性卒中的常见原因。动脉粥样硬化性血栓性卒中患者与其他亚型卒中患者相比,进一步发生血管事件的风险最高,高危患者的年度风险超过15% 。最近的临床试验表明,与常规治疗相比,动脉粥样硬化性血栓性卒中患者可能受益于更强烈的抗血小板疗法或更低的胆固醇低密度脂蛋白(ldl-c)靶向治疗。这意味着这个群体需要更好的、新颖的、量身定做的方法。
二级卒中预防的脂质管理主要目标是使用他汀类药物降低 ldl-c 水平。最近,高甘油三酯水平已成为动脉粥样硬化性心血管疾病的预测指标和新的治疗靶点。甘油三酯富含脂蛋白可进入动脉内膜,促进动脉粥样硬化进程,从而发展成为动脉粥样硬化血栓形成。虽然有相互矛盾的结果,但越来越多的证据表明,使用纤维蛋白或欧米伽 -3脂肪酸来降低甘油三酯的疗法,可能对心血管有潜在的益处。此外,一种新的化合物,可以更有效地降低 tg 水平比目前可用的试剂已经开发和测试,在正在进行的第三阶段试验。
高甘油三酯血症和动脉粥样硬化性血栓性卒中之间的关系研究很少,其预后作用尚不清楚。近日,有研究人员试图评估高甘油三酯血症对动脉粥样硬化性血栓性卒中患者残余心血管风险的影响。
东京女子医科大学卒中登记处是一个持续的前瞻性、观察性的登记处,其中870名急性缺血性卒中或短暂性脑缺血发作,在发病后一周内连续登记并随访一年。高甘油三酯血症定义为空腹血清甘油三酯≥150mg/dl。颈头动脉明显狭窄定义为50% 或更大的狭窄、闭塞。主要结果是主要的不良心血管事件,包括非致命性卒中、非致命性急性冠状动脉综合症和血管性死亡。
- 870例患者(平均年龄70.1岁,男性60.9%)中有217例(24.9%)存在高甘油三酯血症。
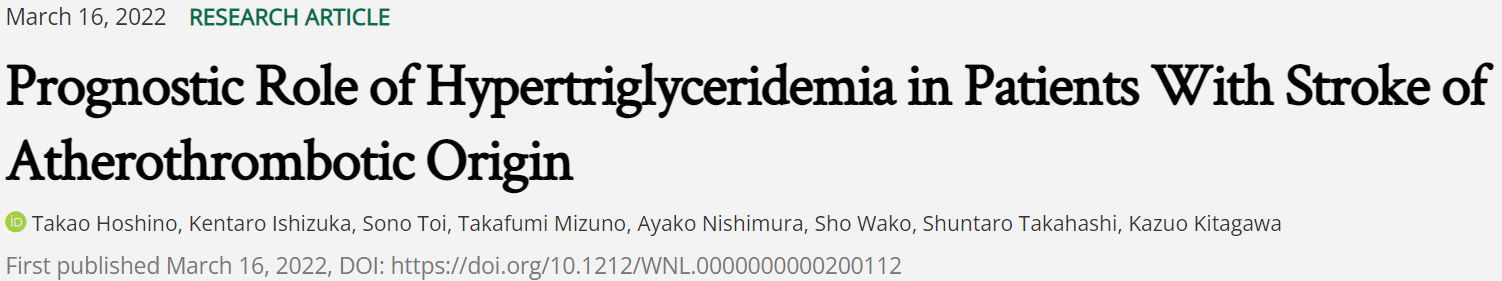
- 高甘油三酯水平与颅内动脉狭窄的发生率增加有显著相关,尤其是在前循环,而不是颅外动脉狭窄。
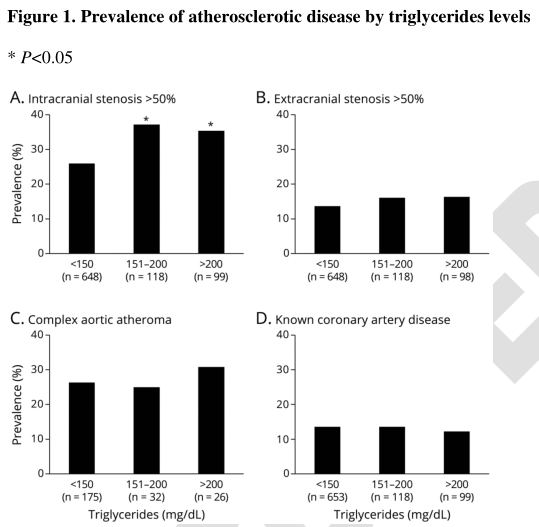
- 即使调整了潜在的混杂因素,包括基线低密度脂蛋白胆固醇和他汀类药物的使用(调整后的危害比为2.46; 置信区间为95% ,1.62-3.74) ,高甘油三酯血症患者发生严重心血管不良事件的风险也高于那些没有发生此类事件的患者(年发生率为20.9% 对9.7% ; p < 0.001)。
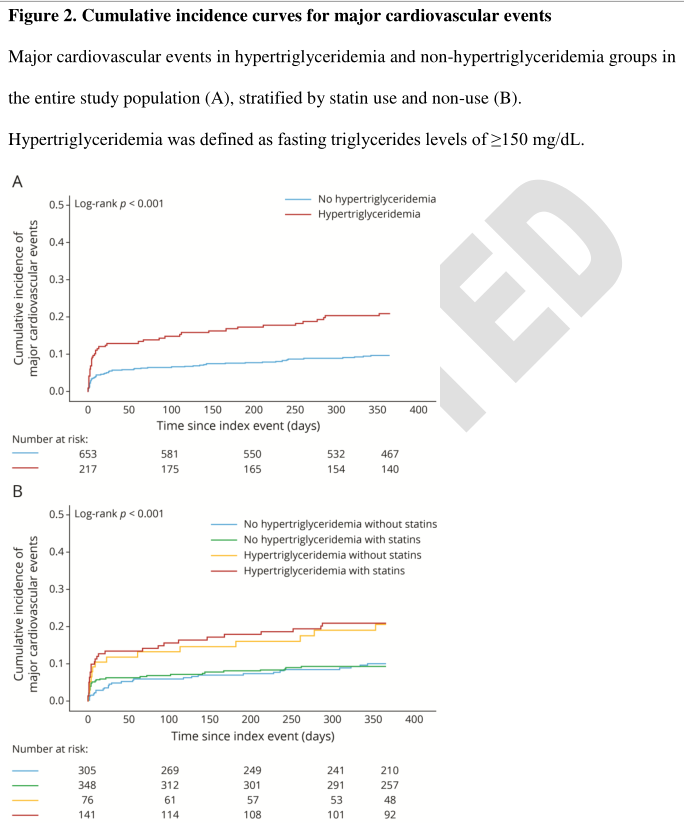
- 高甘油三酯血症患者血管事件发生的危险性高于非高甘油三酯血症患者(n = 174,年发生率35.1% 对14.2% ,p = 0.001) ,颅内动脉明显狭窄者(n = 247,年发生率29.9% 对14.7% ,p = 0.006) ,以及颅外动脉明显狭窄者狭窄(n = 123,年发病率23.0% ,9.4% ,p = 0.042)。
- 与此相反,高甘油三酯血症并不能预测心源性栓塞性卒中患者的复发性血管事件(n = 221; 年发病率19.1% 对10.5% ; p = 0.18)。
高甘油三酯血症是一个重要的可改变的危险因素,促使动脉粥样硬化血栓性卒中患者的残余血管风险,即使在他汀治疗期间。
试验注册信息: 东京女子医科大学卒中登记处的注册 https://upload.umin.ac.jp 是 umin000031913。
这项研究提供了一级证据,证明在动脉粥样硬化血栓性卒中患者中,高甘油三酯血症与主要心血管事件的风险增加有关。
文献来源:Hoshino T, Ishizuka K, Toi S, et al. Prognostic Role of Hypertriglyceridemia in Patients With Stroke of Atherothrombotic Origin [published online ahead of print, 2022 Mar 16]. Neurology. 2022;10.1212/WNL.0000000000200112. doi:10.1212/WNL.0000000000200112
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





















#卒中患者#
121 举报
#血栓性#
133 举报
#粥样硬化#
97 举报
#患者预后#
127 举报
#Neurol#
104 举报
#高甘油三酯#
97 举报
#粥样硬化性#
91 举报
#脑卒中患者#
136 举报
学习了
130 举报
学习了
133 举报