PNAS:致命脑肿瘤的新希望!三氟拉嗪与放射线结合
2020-05-04 Allan MedSci原创
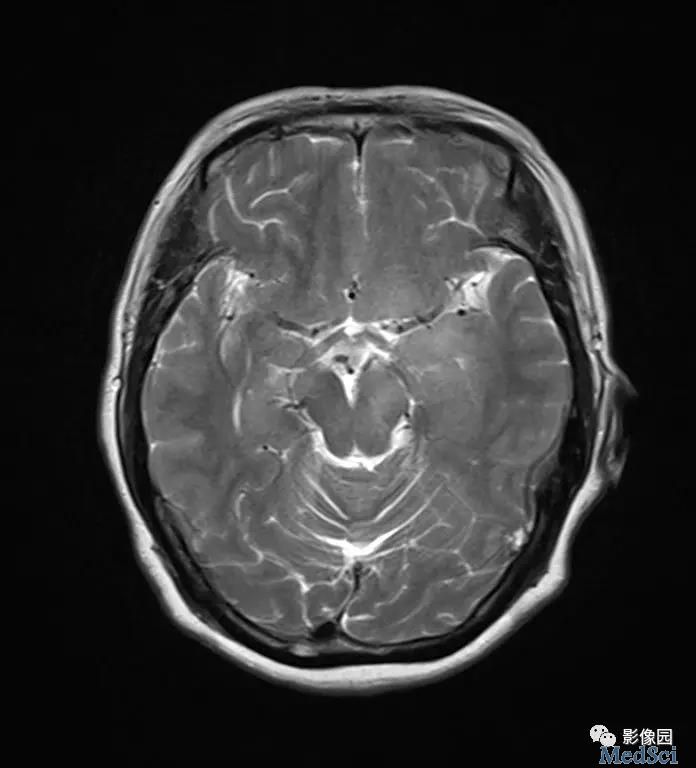
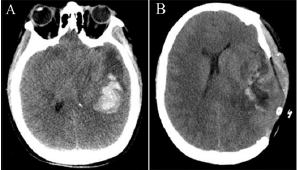
加州大学洛杉矶分校约翰逊综合癌症中心的研究人员发现,将一种曾经用于治疗精神分裂症的药物(三氟拉嗪)添加到传统放疗中有助于改善胶质母细胞瘤小鼠的整体生存。胶质母细胞瘤是最致命,最难治疗的脑肿瘤之一。
加州大学洛杉矶分校约翰逊综合癌症中心的研究人员发现,将一种曾经用于治疗精神分裂症的药物(三氟拉嗪)添加到传统放疗中有助于改善胶质母细胞瘤小鼠的整体生存。胶质母细胞瘤是最致命,最难治疗的脑肿瘤之一。这项发现发表于《美国国家科学院院刊,PNAS》。更重要的是,放射线和三氟拉嗪的结合不仅针对胶质细胞瘤细胞,而且还有助于克服这种侵袭性癌症常见的耐药性。
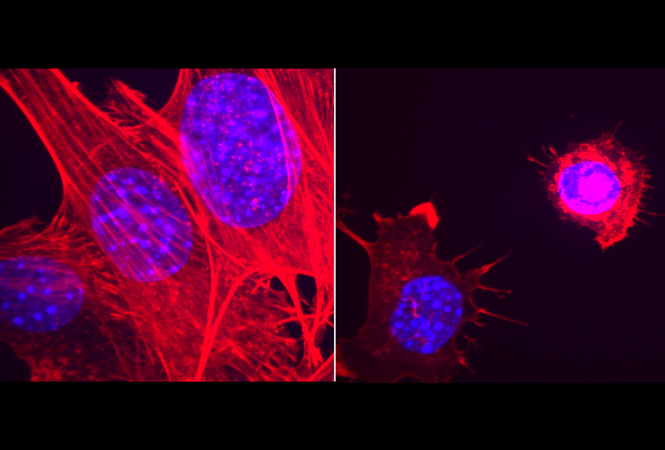
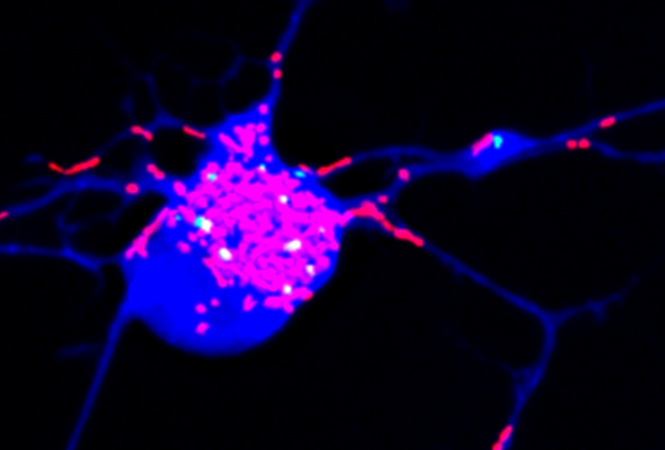
放射线是癌症患者治疗不可或缺的一部分,也是最有效的治疗方法之一。在许多情况下,它可以帮助治愈疾病。但是在胶质母细胞瘤中,肿瘤细胞通常会变得对放射线有抵抗力,因为放射线本身可以诱导“表型转化”,这一过程将某些非肿瘤干细胞转变为产生肿瘤的细胞,从而导致癌症复发。
加州大学洛杉矶分校Frank Pajonk博士说:“虽然放疗是能延长胶质母细胞瘤患者生存的少数疗法之一,但由于高度侵袭性,单独的放疗在我们的模型中对疾病的治疗作用很小。药物三氟拉嗪本身不起作用,但是三氟拉嗪与放射线结合使用时,它们将变得非常高效”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















国内早就有相关文章了。。。。。。
90
#三氟拉嗪#
75
#PNAS#
74
#新希望#
76
#脑肿瘤#
92