自体粒细胞集落刺激因子动员的外周血CD34阳性细胞治疗急性肾损伤:首次人类报道
2021-05-19 Allan MedSci原创
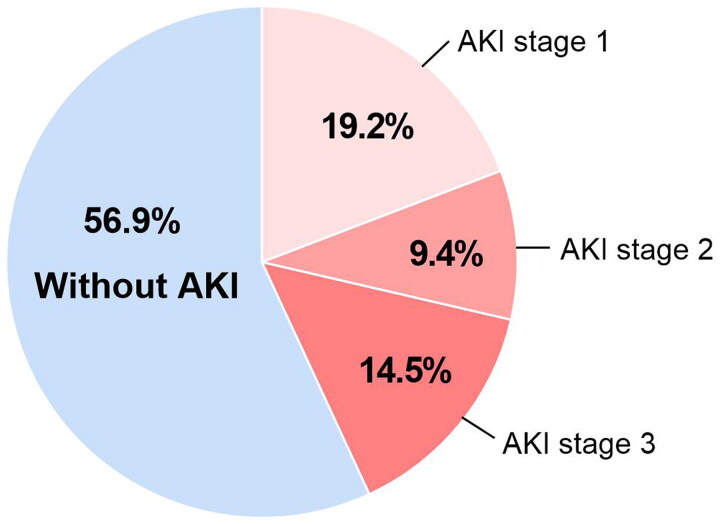
急性肾损伤(AKI)的高患病率及其对重症患者预后的影响是重症监护肾病学领域的主要临床问题之一。
急性肾损伤(AKI)的高患病率及其对重症患者预后的影响是重症监护肾病学领域的主要临床问题之一。尽管在世界许多国家中,严重AKI的死亡率很高(50%或更高),但目前尚无确定的疗法可促进这些患者肾脏的修复。因此,迫切需要一种有效的AKI治疗方法。
研究人员最近报道了在缺血/再灌注AKI动物模型中,富含CD34阳性细胞的人外周血单核细胞移植的功效。细胞疗法可显著改善肾脏功能并恢复由于缺血引起的肾小管周围毛细血管丢失。研究人员已将其他细胞用作再生疗法的来源,包括来自骨髓、脐带、脂肪的间充质干细胞。尽管这些基础研究的结果表明再生疗法可用于AKI,但尚未进行临床试验。
在这里,研究人员介绍了第一例粒细胞集落刺激因子(G-CSF)动员的自体CD34阳性细胞移植用于AKI的情况。
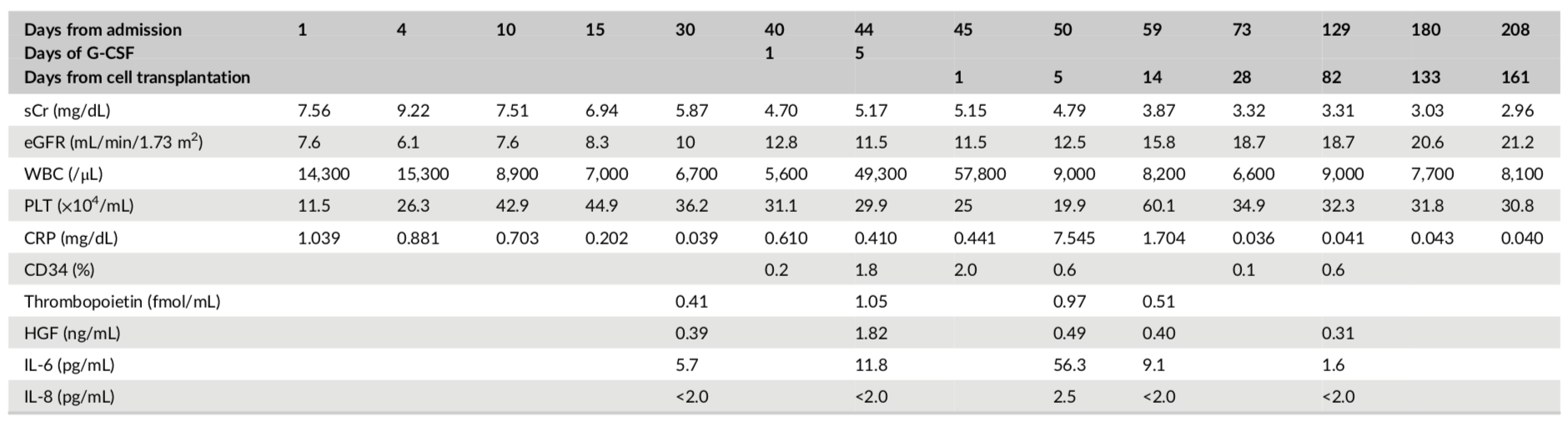
表1 CD34阳性细胞移植前后的实验室检查结果
这是一例患有严重急性肾损伤(AKI)的36岁男子,被送往日本湘南镰仓综合医院。他被诊断为难治性高血压,达到224 / 116mmHg,心电图、眼底镜检查和磁共振成像分别显示出视网膜、心脏和脑部损伤。尽管在通过血管紧张素受体阻滞剂严格控制血压后无需血液透析,但严重的肾功能不全仍然存在。因此,研究人员进行了自体粒细胞集落刺激因子动员的外周血CD34阳性细胞移植。将收集的CD34阳性细胞直接输注到两个肾动脉。细胞治疗后23周血清肌酐水平逐渐提高至2.96 μg/dL。尽管干预后观察到短暂发热和血小板增多,但未观察到重大不良事件。该患者是自体粒细胞集落刺激因子动员的外周血CD34阳性细胞移植治疗严重AKI的I / II期临床试验中的第一例(试验编号jRCTb030190231)。
原始出处:
https://stemcellsjournals.onlinelibrary.wiley.com/doi/full/10.1002/sctm.20-0561
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















学习
133 举报
#损伤#
107 举报
#外周血#
124 举报
学习
148 举报
认真学习了
144 举报
认真学习了
133 举报