阿尔茨海默病(AD)大脑病理的生物标志物被研究、临床试验和记忆诊所用于各种适应症,包括确定认知障碍的病因是否可能与AD或其他原因有关。淀粉样蛋白正电子发射断层扫描(PET)是一种成熟的技术,可以确定一个人是否有明显的脑淀粉样蛋白病,可能导致或促成认知障碍;然而,淀粉样蛋白PET很昂贵,而且可用性有限。脑脊液(CSF)生物标志物也是预测脑淀粉样变的高度准确指标,而且价格较低,但需要熟练的临床医生进行腰椎穿刺(LP)手术,而且一些人认为LP是侵入性的。一些商业化的检测方法可用于测量CSF淀粉样β肽42(Aβ42)、Aβ40、总tau(t-tau)和在181位磷酸化的tau(p-tau181)的浓度,并且已经确定了与脑淀粉样变一致的截止值。
图1: 论文封面图
值得注意的是,脑淀粉样变的生物标志物截止值是在主要由非西班牙裔白人(NHW)组成的队列中定义的,然后适用于所有的人。然而,一些研究发现非裔美国人(AA)的CSF t-tau和p-tau181水平比NHW低,即使调整了年龄、性别、APOE ε4携带者状态和认知障碍等因素。为什么AA人的CSF t-tau和ptau181的水平较低尚不清楚,可能是由于医疗合并症、生物因素或健康的社会决定因素的不同所致。
不管根本原因是什么,这些差异对CSF生物标志物的效用有重要影响。将NHW中定义的生物标志物截止值应用于生物标志物未被研究的群体,有可能使其他群体接受额外的测试、错误的医疗管理、错过用AD特异性疗法治疗的机会,以及降低AD临床试验的注册人数。
然而,根据种族来 "调整 "医学测试的解释也是非常有问题的,特别是考虑到种族群体内部的异质性和种族的动态性质,因为它是一个社会而不是一个生物结构。相反,最好是使用在不同种族和民族群体中表现准确和一致的AD生物标志物。另外,调整AD生物标志物的种族差异的因素(如医疗合并症)可能更有效,并可在各群体中推广。
在过去的三年里,基于血液的AD生物标志物得到了快速发展。由C2N诊断公司提供的PrecivityADTM测试,包括通过质谱法对血浆Aβ42/Aβ40和脂蛋白E(apoE)蛋白型的高度精确测量,现在已可用于临床。多种血浆p-tau异构体也可作为脑淀粉样变的生物标志物,包括p-tau181、p-tau217和p-tau231。
血浆神经丝轻链(NfL)也可作为神经轴突损伤的非特异性标志物。评估这些检测方法是否准确和一致地预测不同种族和族裔群体的脑淀粉样变是至关重要的。
在这项研究中,有CSF生物标志物和淀粉质PET信息的最大的AA队列之一被用来检查这些脑淀粉样变的参考措施与C2N诊断公司PrecivityAD检测血浆Aβ42/Aβ40以及Simoa免疫检测p-tau181、ptau231和NfL的关系。
在记忆和衰老研究中,自认为是非洲裔美国人(AA)的人与自认为是非西班牙裔白人(NHW)的人按年龄、APOE ε4携带者状态和认知状态进行1:1匹配。每个参与者都进行了血液和脑脊液的采集,并对103名参与者(68%)进行了淀粉样蛋白PET检查。血浆Aβ42/Aβ40是通过高性能免疫沉淀-质谱分析法测量的。
血浆p-tau181、p-tau231和NfL由Simoa免疫分析法测量。CSF Aβ42/Aβ40和淀粉样蛋白PET状态分别作为脑淀粉样蛋白病的主要和次要参考标准。
有76对匹配的AA和NHW参与者(n=152)。对于AA和NHW组,中位年龄为68.4岁,42%为APOE ε4携带者,91%认知正常。
通过CSF Aβ42/Aβ40,AA组比NHW组有脑淀粉样变的可能性小(22% vs 43% 阳性;P = 0.003)。CSF Aβ42/Aβ40状态与血浆生物标志物的接收器操作特征曲线下面积如下。
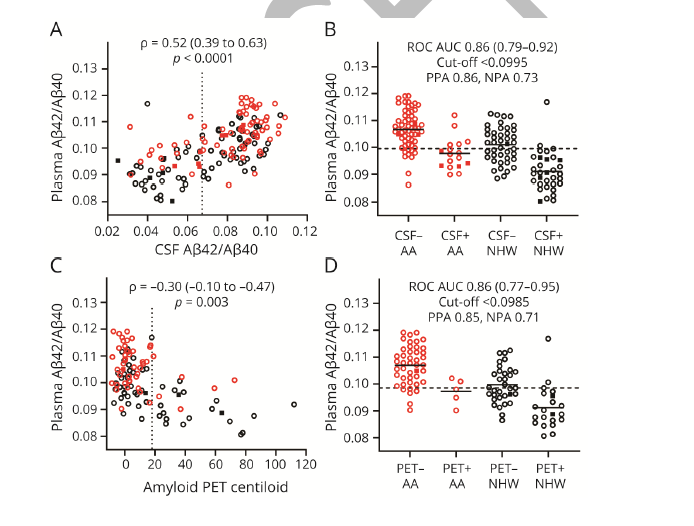
图2:论文结果图
Aβ42/Aβ40,0.86(95% CI 0.79-0.92);p-tau181,0.76(0.68-0.84);p-tau231,0.69(0.60-0.78);和NfL,0.64(0.55-0.73)。
在用血浆Aβ42/Aβ40预测CSF Aβ42/Aβ40状态的模型中,包括协变量(年龄、性别、APOE ε4携带者状态、种族和认知状态),种族并不影响CSF Aβ42/Aβ40阳性的概率。在基于血浆p-tau181、p-tau231或NfL的类似模型中,AA参与者的CSF Aβ42/Aβ40阳性概率较低(几率比分别为0.31 [95% CI 0.13-0.73]、0.30 [0.13-0.71]和0.27 [0.12-0.64])。淀粉样蛋白PET状态的模型也得到了类似的结果。
该研究使用高性能的血浆Aβ42/Aβ40检测方法预测脑淀粉样变的模型,可能提供一个准确和一致的测量AA和NHW组的脑淀粉样变,但基于血浆p-tau181、p-tau231和NfL的模型可能表现不一致,可能导致对AA个体的过度误诊。
原文出处:
Schindler SE, Karikari TK, Ashton NJ, et al. Effect of Race on Prediction of Brain Amyloidosis by Plasma Aβ42/Aβ40, Phosphorylated Tau, and Neurofilament Light. _Neurology_. 2022;99(3):e245-e257. doi:[10.1212/WNL.0000000000200358](https://doi.org/10.1212/WNL.0000000000200358)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#标志物#
122 举报
#脑淀粉样#
124 举报
#神经退行#
109 举报
#Neurol#
94 举报
#淀粉样变#
120 举报