Celltrion收到CHMP对首批推荐用于治疗新冠肺炎的单克隆抗体之一瑞丹维单抗(CT-P59)的肯定意见
2021-11-15 国际文传 网络
Celltrion集团今天宣布,欧洲药品管理局(EMA)人用药品委员会(CHMP)发布了肯定的科学意见,建议向瑞丹维单抗(CT-P59)颁发上市许可。
Celltrion集团今天宣布,欧洲药品管理局(EMA)人用药品委员会(CHMP)发布了肯定的科学意见,建议向瑞丹维单抗(CT-P59)颁发上市许可。瑞丹维单抗是一种单抗药,用于治疗无需辅助供氧但有较高风险转为重症的新冠肺炎的成人患者。CHMP的肯定意见是提供给欧盟委员会(EC)的科学建议,该委员会负责授予产品在欧盟的上市许可。
Celltrion Healthcare医疗和市场部主管HoUng Kim博士表示:“我们已经积累了瑞丹维单抗在治疗感染新冠病毒及其相关变异株(包括毒性较强的德尔塔变异株)的患者方面的安全性和有效性数据。在Celltrion,我们很自豪能在应对新冠肺炎这一前所未有的全球威胁中发挥自己的作用,并相信瑞丹维单抗是对现有治疗方法的重要补充。利用我们稳定的供应体系和商业网络,我们将加快所需流程,并继续与全球利益相关方合作,以确保符合条件的患者能尽快受益于这种治疗方法。目前,我们正在与全球约30个国家的监管机构和公司进行讨论,以便为治疗新冠肺炎提供我们的单克隆抗体,这将是我们未来几个月的首要任务。”
CHMP的肯定意见得到全球III期临床试验数据的支持,在这项试验中,Celltrion在包括美国、西班牙和罗马尼亚在内的13个国家招募了超过1,315例患者,以评价瑞丹维单抗的有效性和安全性。数据显示,对于有较大风险转为重症的新冠肺炎患者,瑞丹维单抗可显著降低新冠肺炎相关的住院或死亡风险,降低幅度高达72%。
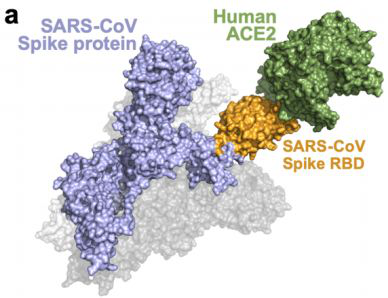
罗马尼亚卡罗尔·达维拉医药大学(Carol Davila University of Medicine and Pharmacy)传染病学副教授Oana Sandulescu, MD博士表示:“单克隆抗体的主要益处是其高特异性和安全性——它们对单一靶点具有高度特异性,因此很少引起不良反应。在新近确诊、未住院的高危人群中,输注一小时瑞丹维单抗这样的单克隆抗体,即可缓解新冠肺炎症状并减少并发症,从而在防止病毒进一步传播方面发挥重要作用。
EMA于今年2月启动了对瑞丹维单抗的滚动审查。在CHMP宣布对瑞丹维单抗的肯定意见之前,Celltrion已于2021年10月向EMA提交瑞丹维单抗的上市许可申请(MAA)。
截至2021年11月,韩国127家医院已有超过21,366例患者接受了瑞丹维单抗治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#CEL#
106
#克隆#
88
#Cell#
75
#Trio#
107
#Celltrion#
70
已阅,受益匪浅。
78
#CHMP#
153