NICE推荐Bavncio (avelumab)治疗局部晚期转移性尿路上皮癌 (UC)
2022-04-17 Allan MedSci原创
Avelumab 组的 1 年总生存率为 71.3%,对照组为 58.4%(P=0.001)。
英国国家健康与护理卓越研究所 (NICE) 建议将免疫疗法 Bavncio (avelumab) 作为符合条件的局部晚期转移性尿路上皮癌 (UC) 成年患者的维持治疗选择。
膀胱癌泛指各种出自膀胱的恶性肿瘤。膀胱是贮存尿液的中空器官,外壁主要由肌肉构成,位于下腹部。罹患膀胱癌最主要的危险因子是来自基因的影响,另外吸烟、长期接触某种染料、汽油或其他化学物质者也有较高的风险。膀胱癌是英国第 11 大常见癌症,也是癌症死亡的第 10 大常见原因。UC 占膀胱癌病例的 90%,生存结果较差。膀胱癌的复发率高达 74% 以上,诊断为四期的患者一年生存率仅为 36%。
NICE 的决定标志着 avelumab 成为第一个也是唯一一个单一疗法,用于在铂类化疗后无进展的局部晚期或转移性 UC 成人患者的一线维持治疗。
一项 III 期试验纳入了无法切除的局部晚期或转移性尿路上皮癌患者。主要终点是总生存期,次要终点包括无进展生存期和安全性。在接受随机分组的所有 700 名患者中,与单独的最佳支持治疗(对照)相比,在最佳支持治疗中添加维持性 avelumab 显著延长了患者总生存期。Avelumab 组的 1 年总生存率为 71.3%,对照组为 58.4%(中位总生存期为 21.4 个月对 14.3 个月;死亡风险比,0.69;95% CI 0.56-0.86; P = 0.001)(图1)。Avelumab 还显著延长了 PD-L1 阳性人群的总生存期。在总体人群中,Avelumab 组的中位无进展生存期为 3.7 个月,对照组为 2.0 个月。Avelumab 组全因不良事件发生率为98.0%,对照组为77.7%;3 级或更高级别的不良事件发生率分别为 47.4% 和 25.2%。
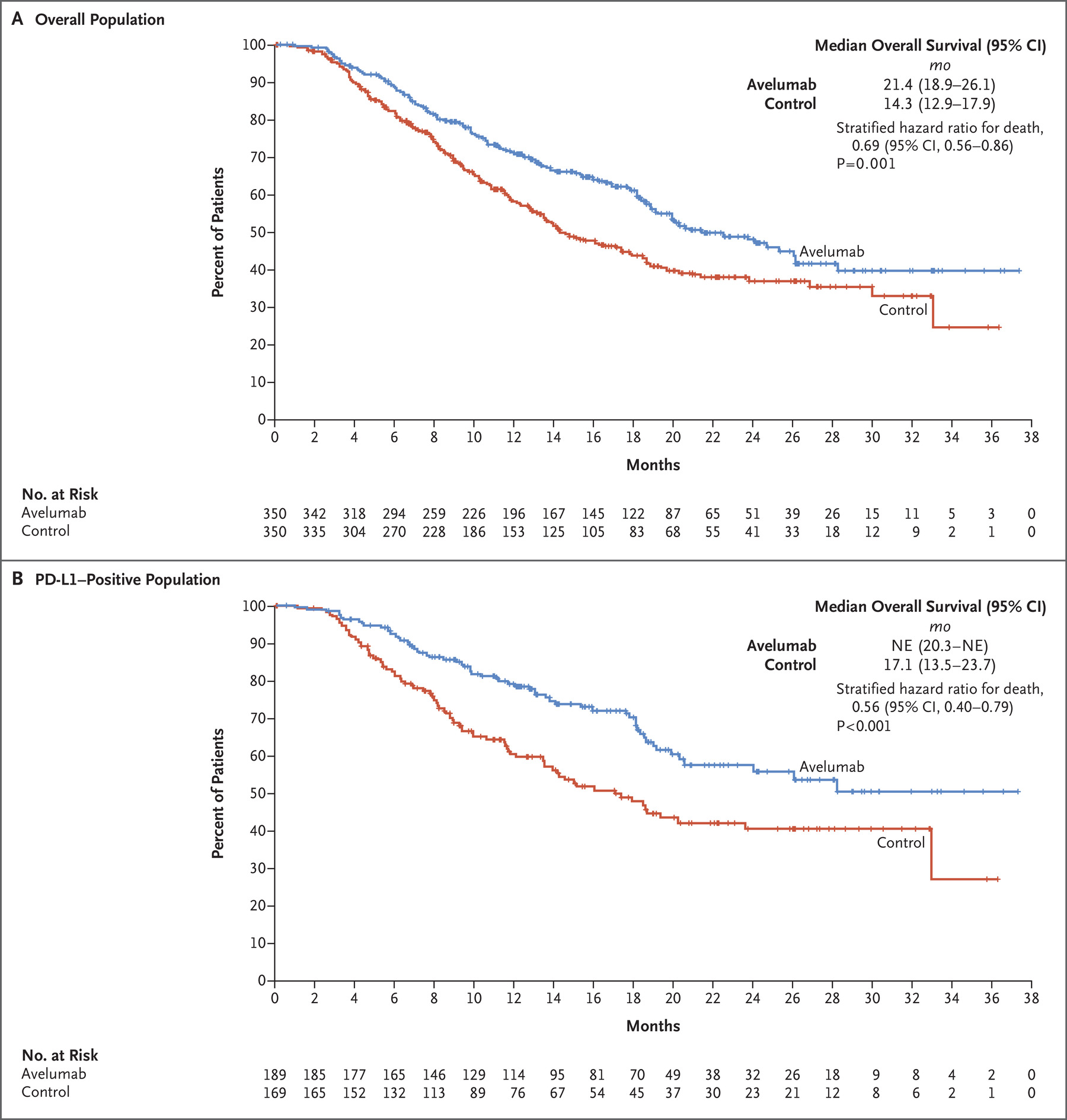
图1. Avelumab 组 vs. 对照组的OS
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#mAb#
75
#局部晚期#
94
#NCI#
83
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
77
#NICE#
110
#avelumab#
84
#转移性#
75
#转移性尿路上皮癌#
84
#局部#
77
#上皮癌#
98