Gut:结直肠病变内镜全层切除术效果评价
2017-08-11 zhangfan MedSci原创
内镜全层切除术具有极高的手术成功率,特别是对于病变小于2cm 的患者,但对于早期肿瘤的根除率尚不理想
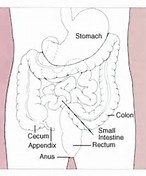
内镜全层切除术(EFTR)是一种结直肠病变的新疗法,可用于某些不适用传统内镜切除法的患者。近日研究人员开展了前瞻性多中心研究,评估全层切除术的有效性和安全性。研究在9个医疗中心开展,招募患者181人,患者存在难治性腺瘤、早期肿瘤或上皮下肿瘤。研究终点是完成手术和R0切除率。内镜全层切除术成功率为89.5%,R0切除率为76.9%,在难治性腺瘤与良性组织学并存的127名患者中,R0切除率为77.7%。在14例疑似癌变和15例确诊癌变患者中,R0切除率达到72.4%,但8例患者存在超过1000μm的深部黏膜下浸润,故根治性切除率为44.8%。对于上皮下肿瘤亚组患者(n=23), R0切除率为87.0%。≤2cm病变患者的R0切除率高于>2cm病变患者(81.2% vs 58.1%,p=0.0038)。不良反应发生率为9.9%,急诊外科发生率为2.2%。对154名患者进行了为期3个月的随访,复发或残留肿瘤发生率为15.3%。内镜全层切除术具有极高的手术成功率,特别是对于病变小于2cm 的患者,但对于早期肿瘤的根除率尚不理想。原始出处:Arthur Schmidt et al. Colo
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
73
谢谢分享,学习了很好!
89
#内镜#
88
#评价#
73
#结直肠#
85
谢谢分享。
0
继续关注。
86
继续学习。
91
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
83
内镜全层切除术具有极高的手术成功率,特别是对于病变小于2cm的患者,但对于早期肿瘤的根除率尚不理想。
64