填补世界空白:阜外医院完成全球首例“完全可降解封堵器”植入术
2018-02-09 佚名 中国循环杂志
2018年2月2日,国家心血管病中心复合技术团队成功完成全球首例“完全可降解封堵器”植入术。
2018年2月2日,国家心血管病中心复合技术团队成功完成全球首例“完全可降解封堵器”植入术。
本次手术由阜外医院外科病房主任、云南阜外医院执行院长潘湘斌教授主刀,在心脏不停跳的情况下,全程采用超声引导,通过仅拇指大小的切口,成功植入全球首例完全可降解室间隔缺损封堵器,标志着中国在完全可降解封堵器领域取得突破性进展,迈入世界领先行列。
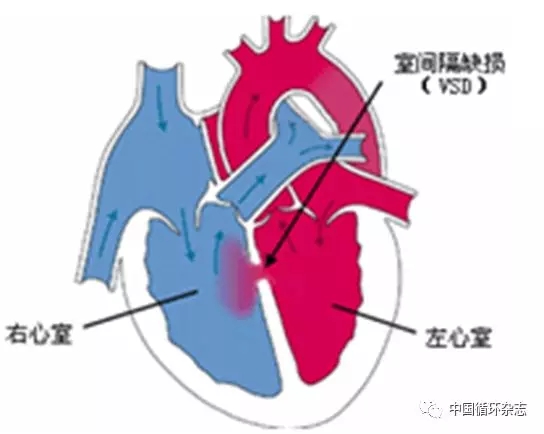
室间隔缺损是一种常见的先天性心脏病(简称先心病),约占先心病的30~50%。正常人的左心室和右心室被室间隔分开,互不相通。
如果在胎儿时期室间隔发育不全而遗留孔洞,使左心室与右心室相通,在心室水平产生左向右的分流,则称为先天性室间隔缺损,如果得不到及时治疗,将严重威胁患者生命。
目前,介入封堵术是先天性心脏病治疗的常用方法之一。虽然具有创伤小的优点,但是植入人体的封堵器将永久存留在患者体内,不但存在远期并发症,而且部分敏感的病人会有慢性炎症,即俗称的“异物反应”。
研制可吸收封堵器是解决上述问题的关键所在,所以在全世界范围内,投入了大量的资金及技术进行研发,但是由于研究难度巨大,而且可吸收材料在放射线下不显影,各国研制的封堵器多带有不可吸收的金属部件,无法完全解决残留问题,目前全球尚没有可吸收封堵器进入市场。
该复合技术团队联合国家心脏病植介入诊疗器械及设备工程技术研究中心(乐普医疗)带着临床问题开展基础研究,再从材料学成果回到临床应用,终于制造出这款具有完全自主知识产权的完全可吸收封堵器,填补了世界空白。
该产品主要设计者潘湘斌教授指出:我们通过近四年的艰苦努力,尝试了数十种改性方案才获得了合适的材料及封堵性能,并通过了严格的动物实验及国家权威部门的检测,而且我们摒弃了传统的放射线引导方式,采用更先进的超声引导方式,为植入完全可吸收封堵器创造了条件。
与传统封堵器相比,完全可降解心脏封堵器植入人体后可逐渐被自身组织所替代,在治疗缺损的同时,实现了体内无异物残留,杜绝了远期并发症。
此次新技术的成功应用对先心病治疗技术的发展具有重要的意义,代表了未来发展的方向,是国家心血管病中心推动产学研协调发展的又一标志性成果。
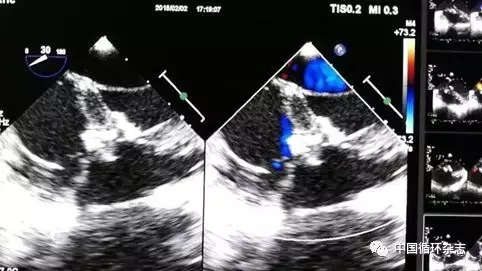
患者术后超声图
这项新技术不仅能造福室间隔缺损患者,还能造福房间隔缺损、动脉导管未闭、心脏瓣膜病、房颤等患者,近期相关产品将逐渐在临床上开展应用,将造福从先天性心脏病到成人心脏病的广大患者。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#全球首例#
86
#解封#
77
#阜外医#
0
#阜外医院#
69
#植入#
78
先进科技.造福人类.非常好
99
学习一下谢谢分享
88
学习了.谢谢分享
1