Mirikizumab达到溃疡性结肠炎研究的主要终点
2021-03-18 Allan MedSci原创
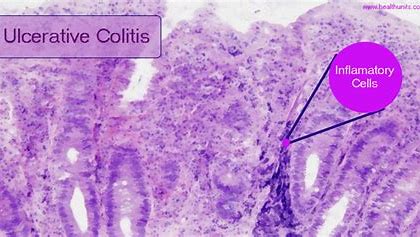
溃疡性结肠炎(UC)是大肠的一种慢性疾病,常常使人衰弱,并影响全球数百万人。UC的症状可能包括血液和粘液引起的慢性腹泻、腹痛和绞痛以及体重减轻。UC可以对工作、家庭和社交活动产生重大影响。
溃疡性结肠炎(UC)是大肠的一种慢性疾病,常常使人衰弱,并影响全球数百万人。UC的症状可能包括血液和粘液引起的慢性腹泻、腹痛和绞痛以及体重减轻。UC可以对工作、家庭和社交活动产生重大影响。
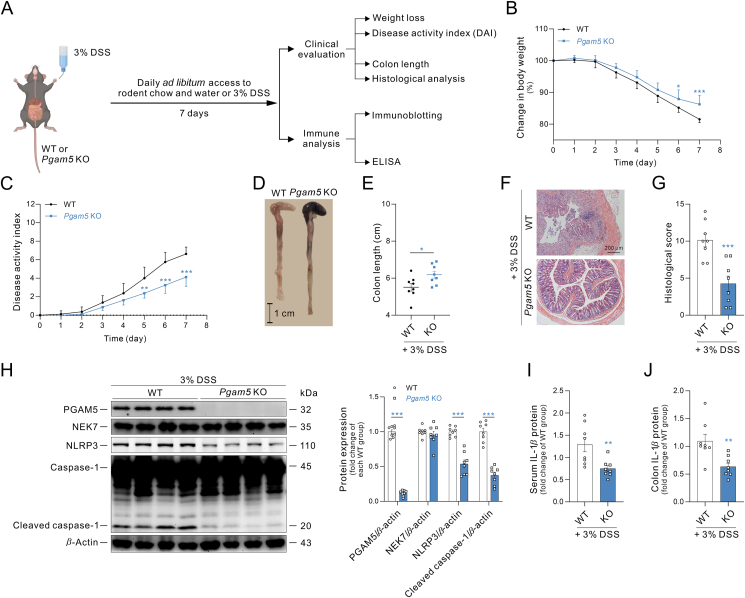
礼来公司的抗IL-23p19单克隆抗体(mAb)mirikizumab在III期溃疡性结肠炎(UC)研究中达到了主要终点和所有关键的次要终点。为期12周的LUCENT-1诱导研究评估了mirikizumab治疗中重度UC患者的有效性和安全性。
在LUCENT-1试验中,与安慰剂相比,mirikizumab在第12周达到了临床缓解的主要终点。这意味着结肠的炎症得到控制或解决,导致症状正常化或接近正常化。此外,mirikizumab在第12周达到了所有主要次要终点,这包括减少肠急症、临床反应、内镜缓解、症状缓解和内镜组织学炎症的改善。
Mirikizumab还在开始治疗后的4周内就表现出患者症状的快速改善,并且减轻了先前对生物制剂或Janus激酶(JAK)抑制剂疗法无反应或已停止反应的患者的症状。
礼来公司免疫学发展副总裁Lotus Mallbris说:“患有UC的人们通常很难有效地控制这种疾病的复发。有了这些积极的结果,我们希望这项研究能够持续52周,以提供更多数据”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#溃疡性#
115
#mAb#
0
#miR#
76
值得学习和借鉴经验!
152
#主要终点#
91
666
167