Endoscopy:重症急性坏死性胰腺炎患者是否应该预防性使用胰管支架置入术?
2020-09-26 MedSci原创 MedSci原创
在急性坏死性胰腺炎(ANP)的患者常见胰管破坏。在这项研究中,我们测试了预防性胰管支架(PPDS)在ANP中的可行性和安全性,并将PPDS与保守治疗进行了比较,研究结果已在线发表于Endoscopy。
在急性坏死性胰腺炎(ANP)的患者常见胰管破坏。在这项研究中,我们测试了预防性胰管支架(PPDS)在ANP中的可行性和安全性,并将PPDS与保守治疗进行了比较,研究结果已在线发表于Endoscopy。
研究人员前瞻性地纳入了2011年2月至2015年7月被诊断为ANP的患者(年龄18 - 75岁)。这些患者在两个三级中心前瞻性地随机接受PPDS或保守治疗。随机化后尽快进行PPDS。
结果,关于PPDS组胰腺坏死的意外感染的担忧促使研究人员进行了中期分析,证实风险高度上升。因此,该试验因伦理原因被提前终止。在PPDS组的11例患者中,所有胰管置入成功的患者(5/5,100%)均出现感染,而保守治疗组13例患者中只有3例(23.1%)出现感染(P=0.01)。分析显示,胰管插管的成功率为63.6%,胰管支架置入的成功率为45.5%,放置支架桥接坏死的成功率为18.2%。插管和支架植入失败的原因是十二指肠水肿和胰管狭窄。
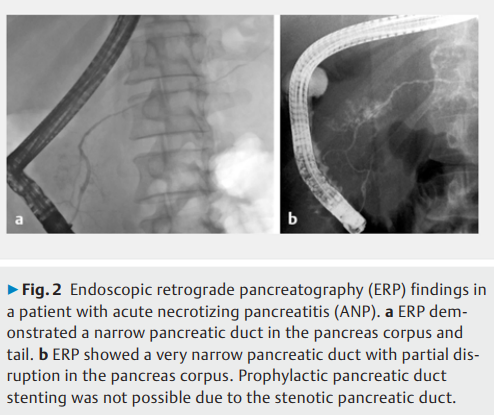
综上所述,该研究结果表明,ANP中的PPDS与不可接受的高胰腺坏死感染风险有关。此外,由于十二指肠水肿和胰管狭窄,该手术在技术上具有挑战性。
原始出处:
Heikki Karjula, Palle Nordblad Schmidt, et al., Prophylactic pancreatic duct stenting in severe acute necrotizing pancreatitis: a prospective randomized study. Endoscopy. 2019 Nov;51(11):1027-1034. doi: 10.1055/a-0865-1960.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








👍
126
#置入术#
103
#预防性#
89
#坏死#
96
#endoscopy#
110