Stroke:血清三甲胺N-氧化物浓度与高血压患者的首次卒中呈正相关
2018-08-21 xing.T MedSci原创
由此可见,较高的TMAO水平与高血压患者中首次卒中的风险增加有关。该研究的结果需要进行精心设计的临床试验来进一步证实,以更好地评估较高TMAO水平对高血压患者预后的影响。
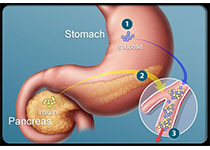
肠源性代谢物三甲胺N-氧化物(TMAO)已被证明是具有致动脉粥样硬化的特性。目前,尚不清楚TMAO是否与首次卒中的风险相关。近日,卒中领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在明确无严重心血管疾病的高血压患者血清TMAO水平与首发卒中之间的关系,并评估任何可能的效应调节因素。
研究人员通过嵌套式病例对照设计,使用来自CSPPT(中国卒中一级预防试验)的数据,包含了622名首次卒中患者和622名匹配对照者。该研究在2008年5月至2013年8月期间进行,其主要结局为首次卒中。
在治疗期间调整胆碱、左旋肉碱和其他重要协变量(包括基线收缩压和时间平均收缩压)后,首次卒中的风险随着TMAO水平的增加而增加([TMAO]每增加1个自然对数比值比为1.22; 95%CI为1.02-1.46)。与血清TMAO水平为最低三分位数(<1.79μmol/ L)的参与者相比,TMAO水平位于第2三分位数(≥1.79μmol/ L;比值比为1.34; 95%CI为1.00-1.81)或TMAO水平位于第3三分位数(≥3.19μmol/ L;比值比为1.43; 95%CI为1.02-2.01)参与者发现首次卒中的风险显著更高。在探索性分析中,研究人员观察到首次卒中时TMAO水平与叶酸水平(≥7.7[中位数] vs. <7.7ng/mL)存在相互作用(相互作用P=0.030)。
由此可见,较高的TMAO水平与高血压患者中首次卒中的风险增加有关。该研究的结果需要进行精心设计的临床试验来进一步证实,以更好地评估较高TMAO水平对高血压患者预后的影响。
原始出处:
Jing Nie,et al. Serum Trimethylamine N-Oxide Concentration Is Positively Associated With First Stroke in Hypertensive Patients.Stroke. 2018. https://www.ahajournals.org/doi/10.1161/STROKEAHA.118.021997
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#正相关#
81 举报
#三甲胺N-氧化物#
81 举报
#高血压患者#
72 举报
#浓度#
81 举报
#三甲#
93 举报
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
88 举报
谢谢分享,学习了
107 举报
学习
144 举报