Alz Res Therapy:胆碱酯酶抑制剂使用,或和认知功能变化无关
2021-11-07 Freeman MedSci原创
在有或没有淀粉样物质负担的患者中,使用或不使用CEI与1年的随访中的认知变化无关
胆碱酯酶抑制剂(ChEIs)是美国食品和药物管理局(FDA)批准的阿尔茨海默病(AD)的对症治疗药物,包括多奈哌齐、利福斯提明和加兰他敏。然而,它们对轻度认知障碍(MCI)的疗效并不确定。根据Petersen等人最近更新的实践指南,在MCI中使用CEI没有A级证据,建议医生可以选择不提供CEI。然而,根据阿尔茨海默病神经影像倡议(ADNI)队列的研究,44%的MCI患者接受了ChEIs治疗。

此前已经进行了相当多的研究来评估CEI治疗对MCI患者的影响。然而,参与者被纳入的依据是MCI的临床诊断,而没有AD的病理学确认。因此,这些研究人群可能包含异质性的病理,这可能导致不一致的结果。
由于缺乏针对MCI患者的经批准的药物治疗,以及对进展为痴呆的担忧,可能导致使用ChEIs,尽管没有强有力的证据证明其疗效。由于ChEIs是基于早期AD的病理变化而开发的,评估ChEIs对有AD生物标志物证实的MCI患者的影响可能为ChEI的使用提供关于开始治疗的时机或治疗的适应症的有用线索。
藉此,韩国首尔大学的的Jung-Min Pyun探究了ChEIs对MCI患者认知能力的影响及其与淀粉样病变的相互作用。
他们纳入了111名临床痴呆评分(CDR)为0.5分的MCI患者,进行了1年的随访认知评估,并在基线认知评估前后6个月内进行了淀粉样蛋白正电子发射断层扫描(PET)(73名CEI使用者和38名CEI非使用者),来自首尔国立大学盆塘医院的神经认知行为中心。
此外,那些在基线认知评估前6个月以上的淀粉样蛋白PET扫描呈阳性的患者和在1年的随访认知评估后6个月以上的淀粉样蛋白PET扫描呈阴性的患者也被纳入。
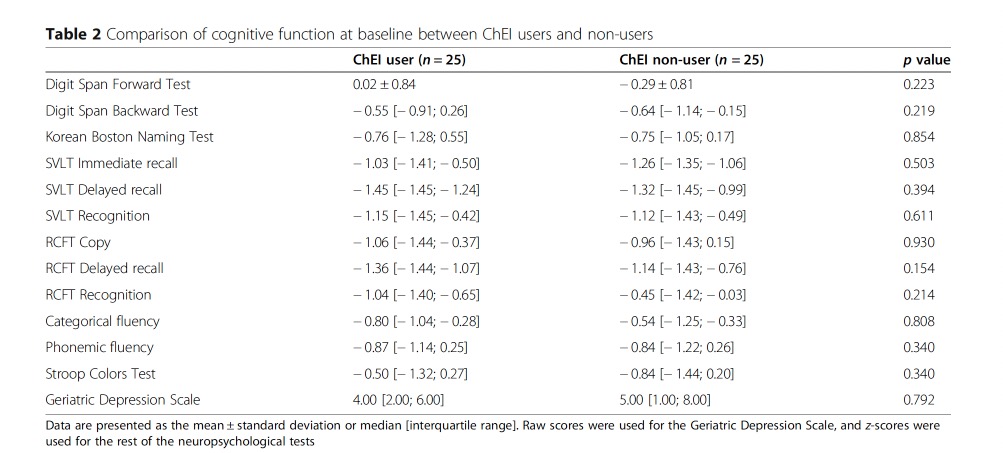
在总共111名患者中,25名CEI使用者和25名CEI非使用者通过基线迷你精神状态检查(MMSE)得分、年龄、教育水平、CDR和淀粉样蛋白PET阳性率进行倾向性评分匹配。进行多元线性回归分析以评估使用CEI和淀粉样PET阳性对1年内认知变化的影响。进行单变量和多变量逻辑回归分析,以评估在1年的随访中,使用CEI和疾病进展到CDR 1之间的关系。
他们发现:使用或不使用CEI与1年内的认知变化没有关系。淀粉样蛋白PET的阳性或阴性并没有改变这种非关联性。
此外,CDR 1的进展与基线MMSE评分低有关(OR 0.606,CI 0.381-0.873),但与使用或不使用CEI无关,也与淀粉样蛋白PET结果无关。
该研究的重要意义在于发现了:在有或没有淀粉样物质负担的患者中,使用或不使用CEI与1年的随访中的认知变化无关。此外,使用或不使用CEI不能预测1年随访时疾病进展到CDR 1。
原文出处:
Pyun JM, Ryoo N, Park YH, Kim S. Change in cognitive function according to cholinesterase inhibitor use and amyloid PET positivity in patients with mild cognitive impairment. Alz Res Therapy. 2021;13(1):10. doi:10.1186/s13195-020-00749-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#ERA#
149 举报
#抑制剂#
111 举报
#胆碱酯酶#
0 举报
#胆碱#
112 举报
学习了!
150 举报