Int J Oral Max Surg:口腔癌术前放化疗对于患者咀嚼、唾液和吞咽功能的重要性:对生活质量的前瞻性研究
2017-09-19 MedSci MedSci原创
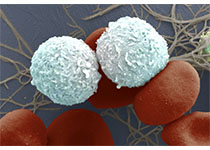
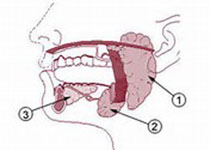
这项研究的主要目的是使用两个经过验证的问卷调查,调查口腔鳞状细胞癌(OSCC)患者接受治疗性新辅助放化疗,之后进行根治性肿瘤切除术,同时口腔重建后的生活质量(QOL)。第二个目标是评估临床变量预测治疗后咀嚼,唾液和吞咽的功能障碍的效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oral#
77 举报
#前瞻性研究#
78 举报
#前瞻性#
91 举报
#吞咽功能#
95 举报
#咀嚼#
138 举报
#重要性#
81 举报
#放化疗#
88 举报
厉害厉害--学习了
123 举报
学习了新知识
105 举报
谢谢分享.学习了
118 举报