Nat Commun: BCL-XL直接调节RAS有利于癌细胞获得干细胞属性
2017-11-02 MedSci MedSci原创
肿瘤组织中,表达高水平抗凋亡蛋白(例如BCL-XL)的化学抗性细胞的积累被认为是在进展和/或初始治疗期间对敏感的低表达克隆进行反选择的结果。本研究中,研究人员发现,即使在没有促凋亡压力的情况下,BCL-XL表达选择性地有利于癌细胞群体。在转化的人乳腺上皮细胞中,BCL-XL有利于组合型活性RAS的下游信号的完全激活,以BH4依赖性的方式相互作用。对比蛋白质组学分析和功能测定表明,这对RAS诱导的干
肿瘤组织中,表达高水平抗凋亡蛋白(例如BCL-XL)的化学抗性细胞的积累被认为是在进展和/或初始治疗期间对敏感的低表达克隆进行反选择的结果。
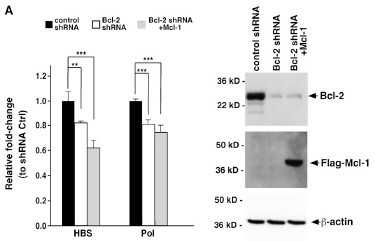
本研究中,研究人员发现,即使在没有促凋亡压力的情况下,BCL-XL表达选择性地有利于癌细胞群体。在转化的人乳腺上皮细胞中,BCL-XL有利于组合型活性RAS的下游信号的完全激活,以BH4依赖性的方式相互作用。对比蛋白质组学分析和功能测定表明,这对RAS诱导的干细胞调节物的表达和维持癌症起始细胞(CIC)表型至关重要。
因此,耐药性癌细胞来自于RAS诱导的自我更新的BCL-XL调节驱动的阳性选择,其中凋亡耐药不一定是直接选择的特征。
原始出处:
Sophie de Carné Trécesson, Frédérique Souazé, et al., BCL-XL directly modulates RAS signalling to favour cancer cell stemness. Nat Commun. 2017; 8: 1123. Published online 2017 Oct 24. doi: 10.1038/s41467-017-01079-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
78 举报
#COMMUN#
73 举报
#癌细胞#
83 举报
#Bcl-xL#
68 举报