Blood:CD19 CAT-T细胞联合依鲁替尼治疗R/R CLL的疗效和安全性
2020-02-22 QQY MedSci原创
中心点:CD19 CAR-T细胞与依鲁替尼同时用于R/R CLL,耐受性良好、CRS严重程度降低和缓解率高。CD19 CAT-T细胞联合依鲁替尼或不联合依鲁替尼的患者的1年PFS分别是38%和50%。摘要:既往研究表明采用CD19 靶向嵌合抗原受体工程T (CD19 CAR-T)细胞免疫治疗复发或难治性(R/R)慢性淋巴细胞白血病(CLL)患者可获得持久的缓解。鉴于预临床研究显示依鲁替尼可提高CA
中心点:
CD19 CAR-T细胞与依鲁替尼同时用于R/R CLL,耐受性良好、CRS严重程度降低和缓解率高。
CD19 CAT-T细胞联合依鲁替尼或不联合依鲁替尼的患者的1年PFS分别是38%和50%。
摘要:
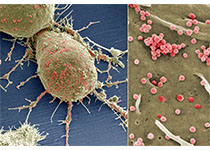
既往研究表明采用CD19 靶向嵌合抗原受体工程T (CD19 CAR-T)细胞免疫治疗复发或难治性(R/R)慢性淋巴细胞白血病(CLL)患者可获得持久的缓解。鉴于预临床研究显示依鲁替尼可提高CAR-T细胞抗肿瘤疗效,减少细胞因子释放综合征(CRS),Gauthier等人开展了一项试点研究,以评估依鲁替尼与CD19 CAR-T细胞免疫治疗联合应用的安全性和可行性。
共招募了19位CLL患者。既往中位治疗次数为5次,17位(89%)患者具有高危细胞遗传学(17p缺失和/或复杂核型)。计划至少在白细胞抽取前2周开始予以依鲁替尼,在CAR-T细胞输注后至少再继续治疗3个月。
依鲁替尼联合CD19 CAR-T细胞免疫治疗的耐受性良好;13位(68%)患者 按计划接受依鲁替尼治疗,未减少药物剂量。4周总体缓解率为83%;61%的患者获得最小残留病灶(MRD)阴性骨髓缓解(IGH测序)。1年总体存活率(OS)和无进展存活率(PFS)分别为86%和59%。与仅采用CAR-T细胞治疗的CLL患者相比,CAR-T细胞联合依鲁替尼可降低CRS的严重程度、降低CRS相关性细胞因子的血清浓度,虽然两种疗法的患者体内有同等的CAR-T细胞扩增。CD19 CAT-T细胞联合依鲁替尼或不联合依鲁替尼的患者的1年PFS分别是38%和50%。
综上所述,CD19 CAT-T细胞联合依鲁替尼治疗R/R CLL的耐受性良好,可降低CRS的严重程度,提高MRD阴性缓解率。
原始出处:
Jordan Gauthier, et al.Feasibility and efficacy of CD19-targeted CAR-T cells with concurrent ibrutinib for CLL after ibrutinib failure.Blood. FEBRUARY 19, 2020
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#疗效和安全性#
109
#CD19#
116
谢谢梅斯提供这么好的信息,学到很多
105