Annals Neurology:临床前期,脑淀粉样血管病白质损伤如何进展?
2022-07-18 Freeman MedSci原创
白质破坏措施可能是D-CAA进展的有价值的横断面和纵向生物标志物
大脑淀粉样血管病(CAA)是一种脑部小血管疾病,是脑内出血的常见原因,也是认知障碍的诱因之一。 尽管大多数CAA病例是散发性的,但淀粉样前体蛋白(APP)的几种遗传变异已被证明可导致常染色体显性形式的CAA。
图1: 论文封面图
最常见的类型是荷兰型CAA(D-CAA),它是由APP的一个点突变(E693Q5)引起的。与散发性CAA相比,D-CAA出现症状的年龄较小,但其临床和放射学表现与散发性CAA相似。
由于其发病年龄早且完全穿透,对D-CAA的研究为了解无症状前CAA的病理生理学提供了一个独特的窗口。
D-CAA是一种致命的孤儿疾病,很少有集中的临床试验。这部分是由于在脑出血出现之前的早期阶段,很难确定合适的疾病进展的生物标志物。
哈佛大学的Zahra Shirzadi等先前的横断面工作表明,白质破坏可能发生在D-CAA的症状性出血之前,他们研究了D-CAA患者纵向队列中白质变化的进展情况。
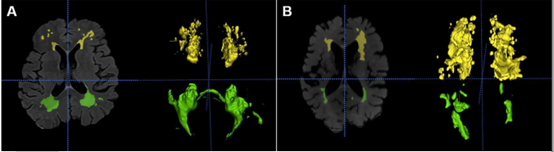
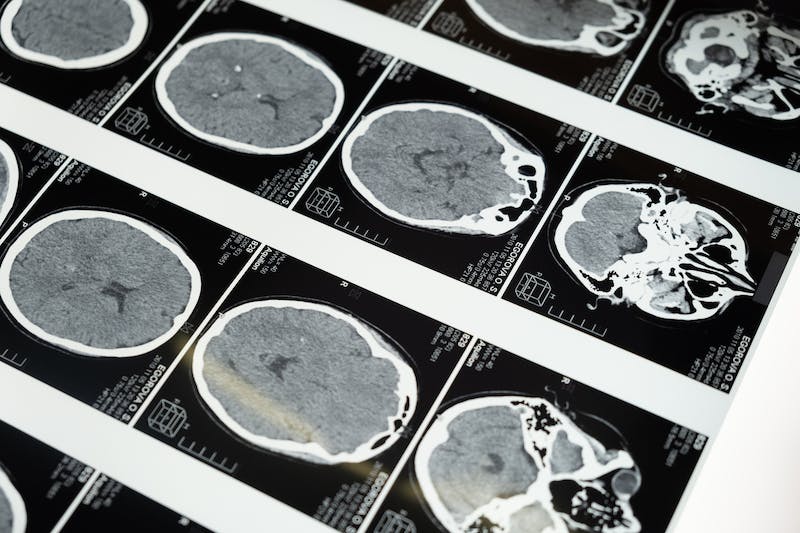
为了研究白质的变化,他们使用了白质超强度(WMH)体积和骨架化平均扩散性(PSMD)的峰值宽度--这是最近开发的基于扩散的测量方法,对脑血管损伤敏感。
 图2:论文结果图
图2:论文结果图
核心假设:在出血性病变或有症状的出血之前,白质损伤的神经影像学措施在D-CAA中是存在的并且是渐进的。
在一个D-CAA携带者和非携带者的纵向队列中,他们观察到D-CAA携带者和非携带者,在出现脑微出血之前,以及在第一次有症状的出血的平均年龄之前>14年,白质损伤措施出现区别。
这些结果表明,白质破坏措施可能是D-CAA进展的有价值的横断面和纵向生物标志物。
原文出处:
Shirzadi Z, Yau WW, Schultz SA, et al. Progressive White Matter Injury in Preclinical Dutch Cerebral Amyloid Angiopathy. _Annals of Neurology_. Published online June 25, 2022:ana.26429. doi:[10.1002/ana.26429](https://doi.org/10.1002/ana.26429)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#血管病#
152
#白质#
137
#脑淀粉样#
123
#Neurol#
117
#损伤#
112
#脑淀粉样血管病#
173