男性,73岁,3个月前他的私人医生发现其舌背部出现一些异常的剥脱性病变。

据该男子主诉,其以往有吸烟史,曾因患有高血压、高胆固醇血症和高尿酸血症进行过治疗。
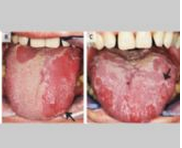
口腔检查可见,在舌背部可观察到圆形的红色的区域,在舌头处也可见一大块的斑块(如图A所示)。会诊医师根据该患者的临床症状诊断其为地图舌,又称为游走性舌炎。
地图舌,在国际上受影响的总人口约达2%,主要是由于局部的炎症及丝状乳头分化不良导致。患有地图舌的患者通常会出现移动性的椭圆形红色区域,在红色区域的周边会有明显的白色边缘。
对于本案例中的患者,在后续的随访中,8个月和20个月时亦可见到明确的白色的边缘(如图B和图C所示)。
一般情况下,患有地图舌的患者是不会出现任何特殊的异常症状的,但当患者在吃辛辣或酸性的食物时容易引发疼痛或灼烧感。当地图舌患者不表现出症状时,可不作任何的治疗。但在32个月内,仍需不定时地进行跟踪随访。
原始出处:
Elena Varoni, Sem Decani,Geographic Tongue,N Engl J Med 2016; 374:670February 18
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







好文章,还会关注
125
赞一个!好文章拜读学习了。
130
知识一点一点的积累了
149
可以学到很多
163