英国药品和保健品监管局 (MHRA) 支持默克的MET抑制剂Tepmetko治疗非小细胞肺癌 (NSCLC)
2021-10-14 Allan MedSci原创
近日,英国药品和保健品监管局 (MHRA) 有条件地授权默克 (Merck) 的MET抑制剂Tepmetko (tepotinib) 用于治疗某些非小细胞肺癌 (NSCLC) 患者。
近日,英国药品和保健品监管局 (MHRA) 有条件地授权默克 (Merck) 的MET抑制剂Tepmetko (tepotinib) 用于治疗某些非小细胞肺癌 (NSCLC) 患者。
非小细胞肺癌最常见于年龄较大的吸烟者和既往吸烟者。肺部的小肿瘤通常无症状,所以多数患者在诊断时存在局部晚期或转移性病变。
Tepmetko有条件的上市许可为携带间充质-上皮转化因子基因外显子14(METex14) 跳跃突变的晚期 NSCLC成年患者提供治疗。
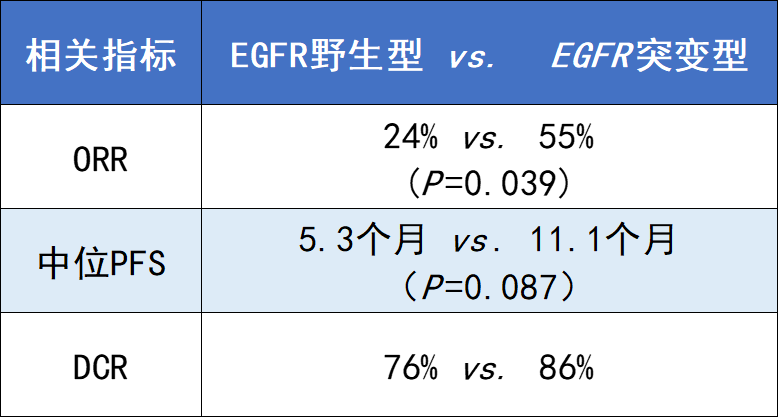
MHRA的决定是基于II期VISION研究的结果,该研究评估了Tepmetko单药治疗具有METex14跳跃突变的晚期或转移性NSCLC患者的有效性,截至2020年1月1日,共有152名患者接受了Tepmetko治疗,其中99名患者的随访时间至少为9个月。在146名患者中评估了Tepmetko的疗效,该研究通过独立审查表明联合活检组的总体缓解率 (ORR) 为45.2%(95% 置信区间 [CI],36 至 57),中位反应持续时间为11.1个月;液体活检组66例患者的ORR率为48%(95% CI,36 至 61);组织活检组60例患者的ORR率为50%(95% CI,37 至 63);研究人员评估的缓解率为56%(95% CI,45 至 66),无论之前接受过针对晚期或转移性疾病的治疗,缓解率都相似(图1)。
28%的患者报告了研究人员认为与tepotinib治疗相关的3级或更高级别的不良事件,包括7%的外周水肿。不良事件导致11%的患者永久停用tepotinib。
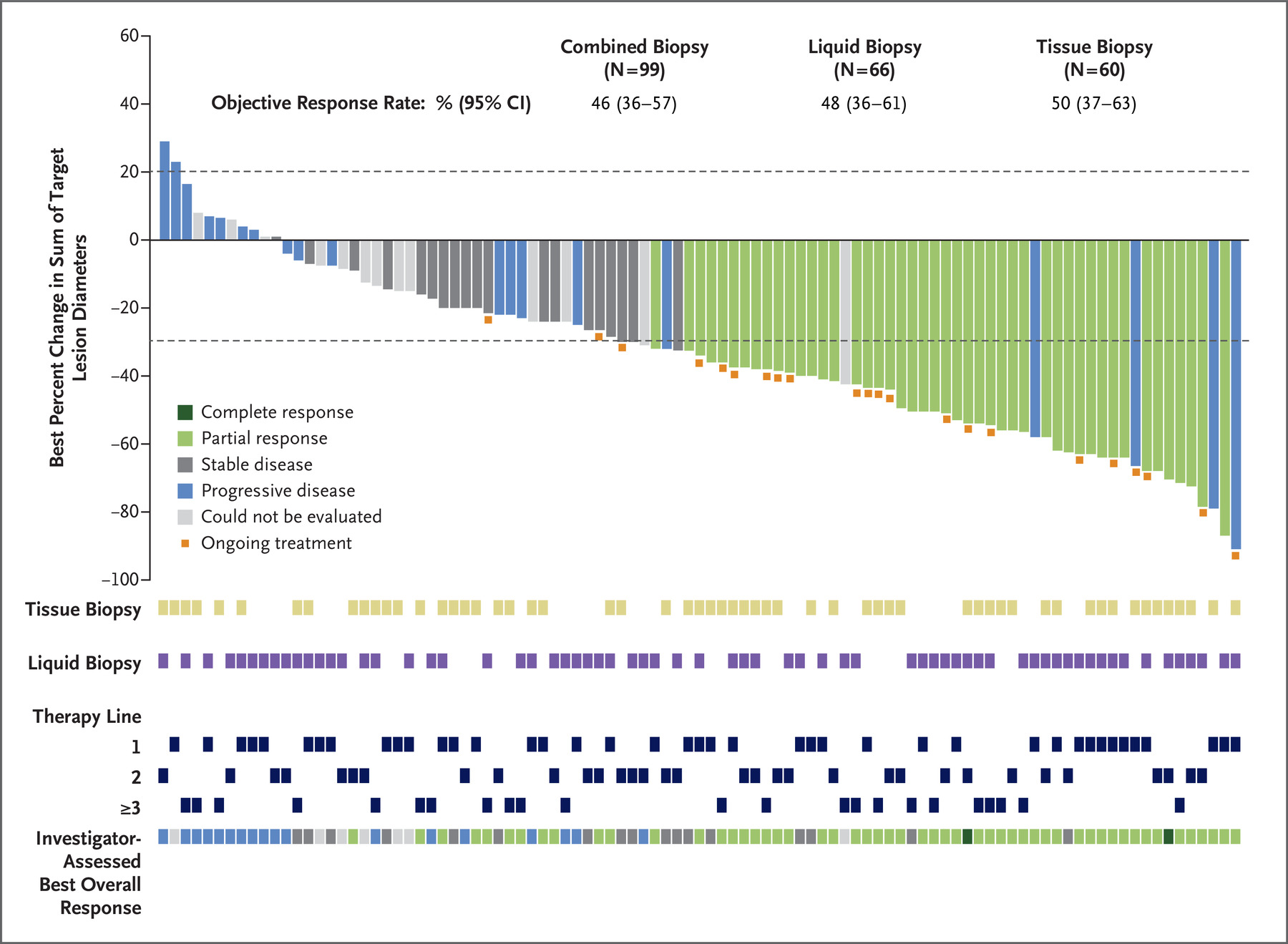
图1.总体缓解率 (ORR)
肺癌基金会Roy Castle首席执行官Paula Chadwick说:“我们欢迎MHRA决定批准靶向疗法tepotinib。肺癌可能是一种侵袭性的、难以治疗的癌症,因此我们必须为患者提供尽可能多的治疗选择,这样他们才能尽可能长时间地与这种疾病一起生活”。
原始出处:
http://www.pharmatimes.com/news/mhra_backs_mercks_met_inhibitor_tepmetko_1380739
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MET抑制剂#
85
#MET#
78
#抑制剂#
75
#非小细胞#
97
#默克#
98
#监管#
107
#Tepmetko#
81