Neurology:影响WHO II级脑胶质瘤术后妊娠妇女长期生存的因素
2022-04-28 Naomi MedSci原创
患WHO II级胶质瘤(GIIG)的妇女常困惑于怀孕对肿瘤预后的影响。研究发现,肿瘤残留量和肿瘤生长速度是制约GIIG患者孕后长期生存的有力预测因素,识别风险患者对有受孕计划GIIG妇女至关重要。
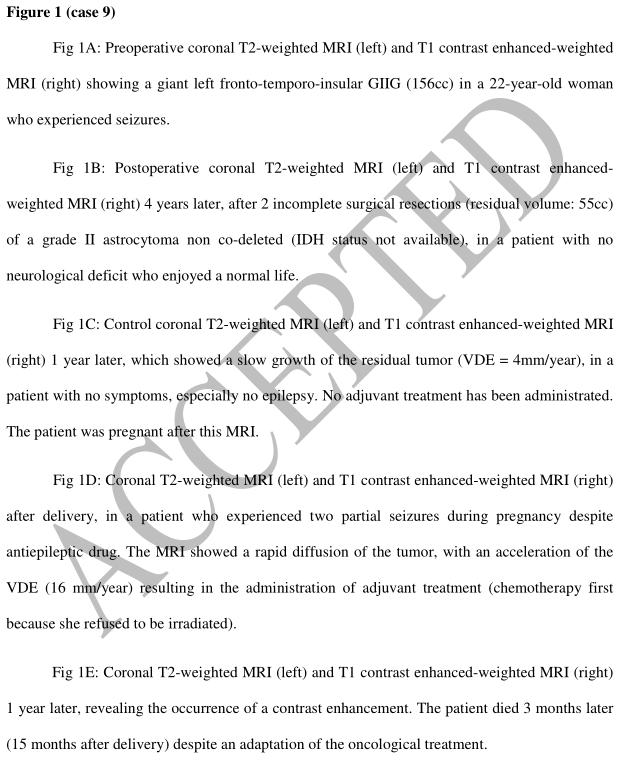
得益于对世卫组织II级胶质瘤(GIIG)采取了积极的治疗策略,特别是依赖于早期最大安全手术,患者预期寿命现在显著延长,最近一系列的总生存期(OS)超过16年。此外,患者生活质量基本保持不变,使正常的家庭、社会和专业活动得以开展。因此,GIIG患者希望进行越来越多的长期人生规划,包括生孩子。然而,当前尚存在争议,若干研究表明怀孕可能会促进胶质瘤的进展和早期临床恶化。然而,除了这些研究是回顾性的之外,还结合了GIIG和高级别胶质瘤、混合了诊断时和诊断后怀孕的患者,并包括经治疗和未治疗的患者,且没有详细说明产后的长期随访。
近日,研究人员连续报告了一系列同种诊断的女性患者,她们在手术切除GIIG后怀孕,在怀孕前未进行肿瘤治疗,且健康状况稳定,即肿瘤没有或生长缓慢、没有对比剂增强、癫痫得到控制。基于围孕期临床放射学预后和妊娠后相关的长期肿瘤学预后的分析,研究人员试图寻找生存的预测因素,以便识别处于危险中的患者,并相应地建议GIIG妇女有成为母亲的愿望。
纳入标准为GIIG切除后已怀孕且怀孕时肿瘤状态稳定(没有正在进行的肿瘤治疗、没有对比剂增强、没有衰弱的临床情况)的成年妇女。相关案例是从其科手术切除的组织学证实的GIIG患者的数据库(1998-2021年)中发现。
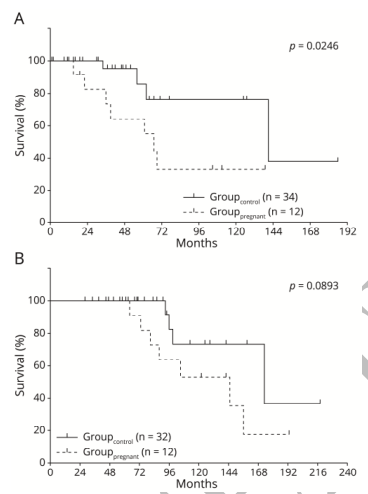
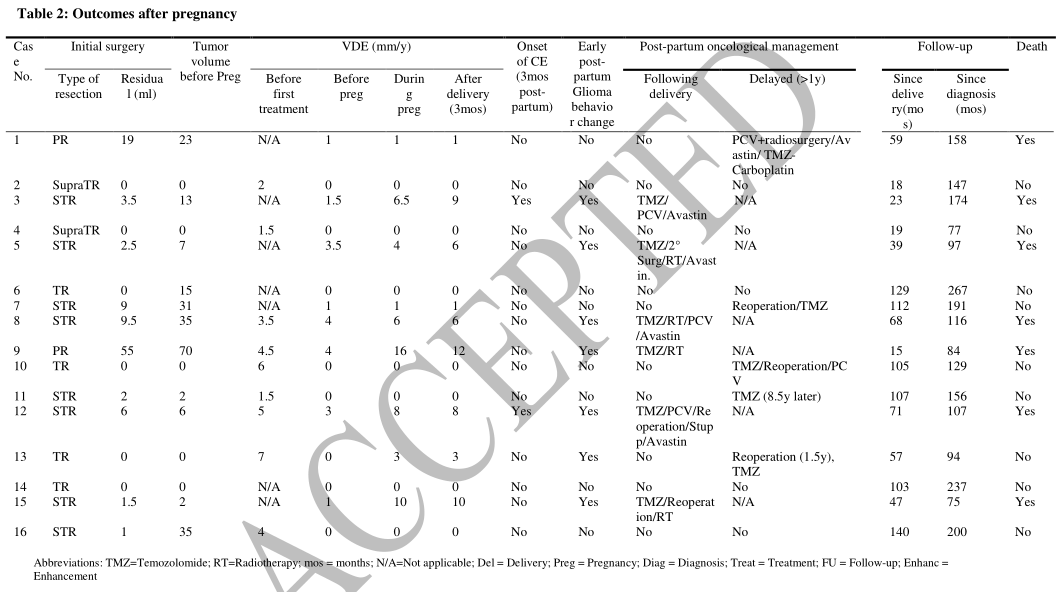
- 345例GIIG育龄妇女(年龄<45岁)中,妊娠16例(4.6%,平均分娩年龄30.9±5.1岁),其中2次妊娠5例。
- 最后一次肿瘤治疗(11例单纯手术,5例化疗和/或放射治疗)到怀孕的平均间隔为3.5年(0.75-10年)。两名患者在怀孕期间癫痫发作。除1例(1例剖腹产)外,其余均为阴道分娩。所有儿童都有正常的心理和身体发育。
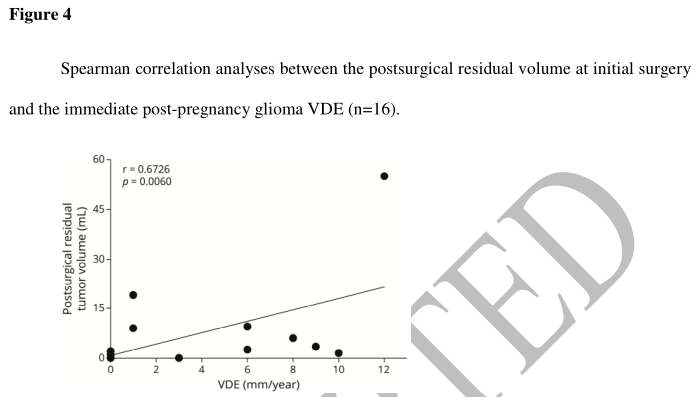
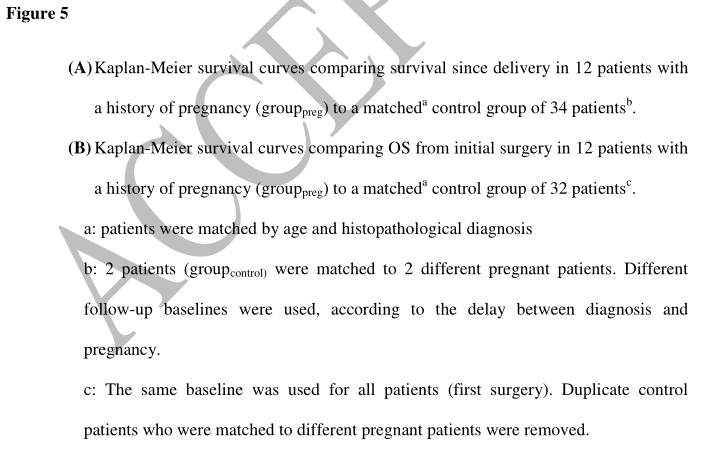
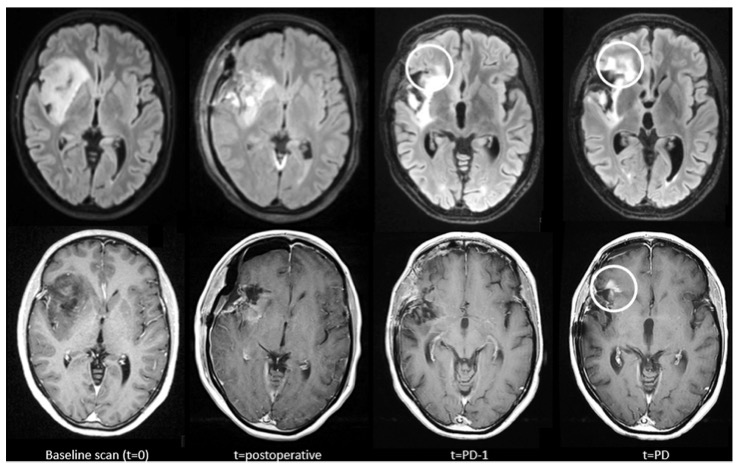
- 7例(43.7%)患者的行为发生改变,直径扩张速度(VDE)加快和/或在孕期或孕后3个月内出现对比剂增强,7例在产后早期接受治疗和/或再次手术。
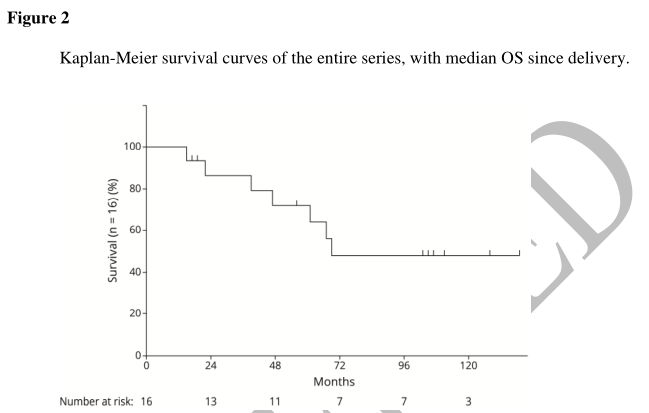
- 分娩后的中位临床随访期为5.3年(1.25~11.6年)。另外4名患者接受了胶质瘤进展的延迟辅助治疗。7例(43.7%)死亡,中位分娩时间为3.9年(1.25-5.9年)。总体而言,分娩后的中位生存期为5.75年。
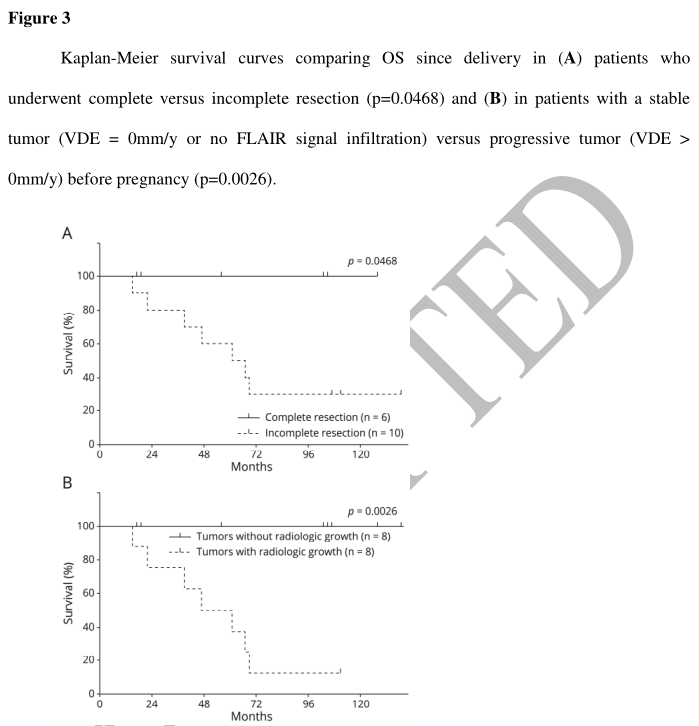
- 至关重要的是,接受过完全手术切除的患者和怀孕前病变稳定的患者的寿命更长(对数等级,分别为p=0.046和p=0.0026)。
肿瘤残留量和肿瘤生长速度是制约GIIG患者孕后长期生存的有力预测因素。识别有风险的患者对于向渴望成为母亲的GIIG妇女提供相关咨询至关重要。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Neurol#
72
不错,学习了。
0
#学习#嗯
0
#长期生存#
91