JAMA Neurology:阿尔茨海默病患者8种血浆淀粉样蛋白Aβ42/40检测方法的比较
2021-11-15 Naomi MedSci原创
检测阿尔茨海默病(AD)中淀粉样蛋白(Aβ)病理是生物标记物在临床治疗中实施的一个重大进步。某些基于高精度免疫沉淀-耦合质谱法的方法在检测脑Aβ病理时比大多数血浆Aβ42/40免疫分析方法表现更得更好
检测阿尔茨海默病(AD)中淀粉样蛋白(Aβ)病理的LOOD测试将是生物标记物在临床治疗中实施的一个重大进步,并在药物试验中非常有用。血液中Aβ的可靠测量被证明是具有挑战性的,直到先进的质谱和免疫检测方法的发展。在2016年,用超灵敏的SIMOA免疫测定法评估的血浆Aβ42/40被证明能以中等准确度检测异常的脑脊液β或β正电子发射断层扫描。高精度免疫沉淀-耦合质谱法(IP-MS)测定的血浆Aβ42/40后来被报道与β-PET相关,并与高精度的脑Aβ负荷异常或将来转为β-PET阳性的高风险个体相鉴别。不同的Aβ分析和平台在整个研究中的不同表现可能部分是由于队列特征(例如,样本大小、纳入的诊断组和结果测量)和分析前样本处理的差异。为了最大限度地减少这些偏倚,近日有研究人员对瑞典BIOFINDER研究中的同一组早期AD患者进行了8种Aβ检测方法的一一比较,以评估了不同方法测定的血浆Aβ42/40与正常脑脊液Aβ42/40或Aβ-PET状态的鉴别能力。
这项研究包括182 BIOFINDER队列中认知正常的参与者和104名轻度认知障碍的患者,他们在瑞典3家不同的医院登记,从2010年到2014年接受了β正电子发射断层扫描、脑脊液和血浆采集。
采用华盛顿大学开发的免疫沉淀耦合质谱法(IP-MS-WASU)、Araclon公司开发的无抗体液相色谱质谱(LC-MS-ARC)和罗氏诊断公司(IA-ELC)、欧洲免疫学公司(IA-EI)、阿姆斯特丹大学医学中心、ADX神经科学公司和Quanterix公司的免疫分析法(IA-N4PE)测定血浆Aβ42/40。用岛津的IP-MS法(IP-MS-SHIM)和哥德堡大学的IP-MS-UGOT法(IP-MS-UGOT)和Quanterix公司的免疫测定法(IA-Quan)分别测定了2 0 0名受试者的血浆Aβ42/40。
为了验证,来自阿尔茨海默病神经成像计划的12名参与者(51名认知正常,51名轻度认知障碍,20名AD痴呆)接受了Aβ-PET和血浆Aβ评估,使用IP-MS-WASU,IP-MS-SHIM,IP-MS-UGOT,IA-ELC,IA-N4PE和IA-Quan分析。
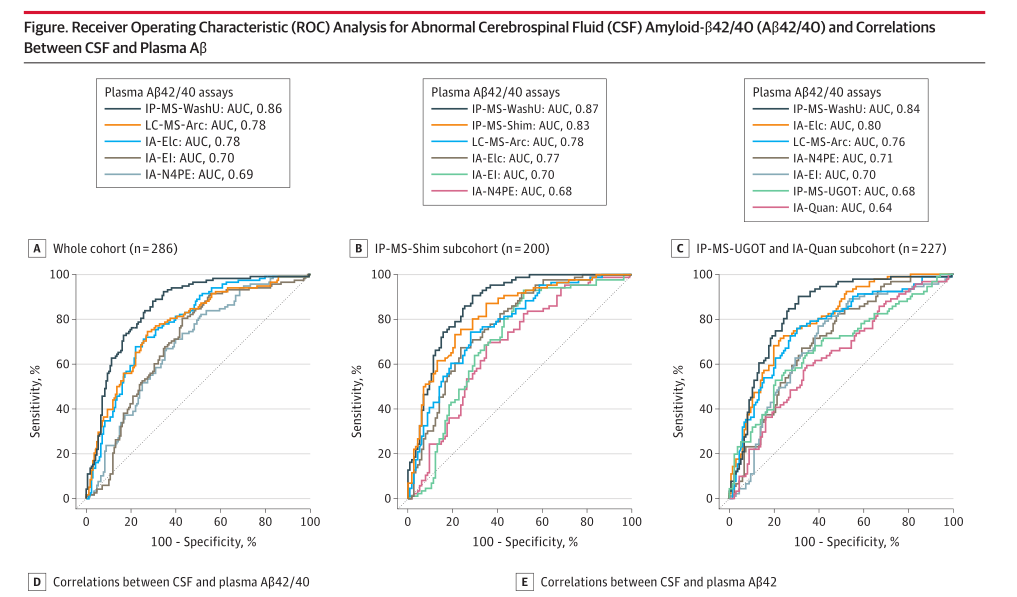
8种不同方法定量检测血浆A-β42/40对异常脑脊液A-β42/40和A-β-PET42/40状态的判别准确性
- 共有408名参与者参与了这项研究。
- 在BioFINDER队列中,平均年龄(SD)为71.6(5.6)岁,其中49.3%为女性。
- 血浆IP-MS-WASU Aβ42/40与LC-MS-Arc Aβ42/40、IA-EI Aβ42/40和IA-N4PE Aβ42/40的准确性(受试者工作特征曲线下面积分别为0.86和0.81~0.90)相比,差异有统计学意义(P<0.05)。
- 血浆IP-MS-WASU Aβ42/40显著优于IP-MS-UGOT Aβ42/40和IA-QUAβ42/40(AUC0.84vs0.68和0.64;P<0.001),而IP-MS-WASU Aβ42/40和IP-MS-Shim Aβ42/40的AUC无明显差异(0.87vs0.83;P=0.16)。
- 当使用Aβ-PET作为结果时,结果是相似的。
- 血浆IPMS-WASU Aβ42/40和IPMS-Shim Aβ42/40与脑脊液Aβ42/40的相关系数最高(r=0.56~0.65)。
- BioFINDER的结果在阿尔茨海默病神经成像倡议队列(平均[SD]年龄,72.4[5.4]岁;43.4%的女性)中得到了复制,其中IP-MS-WASU检测的表现明显优于IP-MS-UGOT、IA-ELC、IA-N4PE和IA-Quan检测,但IP-MS-Shim检测没有。
两个独立队列的结果表明,某些基于MS的方法在检测脑Aβ病理时比大多数血浆Aβ42/40免疫分析方法表现得更好。
文献来源:https://jamanetwork-com.washington.80599.net/journals/jamaneurology/fullarticle/2784411
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#Aβ42#
125 举报
#Neurol#
111 举报
#阿尔茨#
119 举报
#阿尔茨海#
105 举报
#淀粉样蛋白#
123 举报
#检测方法#
132 举报
#阿尔茨海默#
86 举报
#Aβ#
108 举报