J Am Coll Cardiol Intv:紫杉醇涂层球囊治疗长股腘动脉疾病疗效优
2016-05-17 Seven L MedSci原创
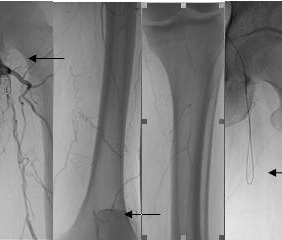
研究者进行了一项研究,评估经皮使用紫杉醇涂层球囊治疗长股腘动脉病变患者的1年结局情况。该多中心研究纳入了Rutherford分类为2-4的患者,其股动脉病 >15 cm,且血管直径4-7 mm。主要研究终点为12个月时的血管通畅率;次要终点包括主要不良事件(复合目标包括死亡、截肢、靶病变部位血栓形成或临床驱动的非靶病变靶血管血运重建)、Rutherford分类改变、踝肱指数和术后24个月患者
研究者进行了一项研究,评估经皮使用紫杉醇涂层球囊治疗长股腘动脉病变患者的1年结局情况。
该多中心研究纳入了Rutherford分类为2-4的患者,其股动脉病 >15 cm,且血管直径4-7 mm。主要研究终点为12个月时的血管通畅率;次要终点包括主要不良事件(复合目标包括死亡、截肢、靶病变部位血栓形成或临床驱动的非靶病变靶血管血运重建)、Rutherford分类改变、踝肱指数和术后24个月患者的生活质量情况。
最终研究纳入了105名患者(平均年龄为68 ± 9岁,81.9%为男性),进行了紫杉醇涂层球囊和临时支架植入术治疗,并且全部获得成功。研究中平均治疗的病变长度为251 ± 71 mm,包括63.4%的中度至重度钙化病变和49.5%的完全闭塞病变。救助支架率达10.9%。有101名(96.2%)患者随访了12个月,84名(83.2%)患者在12个月后血管仍然通畅,7名(6.2%)患者发生了主要不良事件,Rutherford分类变化显示出了显著的临床益处。
研究结果表明,对长股腘动脉疾病患者使用经皮血管内紫杉醇涂层球囊治疗,将取得较好的疗效。
原始出处:
Antonio Micari, Giuseppe Vadalà,et al.1-Year Results of Paclitaxel-Coated Balloons for Long Femoropopliteal Artery Disease.J Am Coll Cardiol Intv. 2016;9(9):950-956. doi:10.1016/j.jcin.2016.02.014
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Coll#
62
#Cardiol#
61
#球囊#
57