Lancet子刊:RET抑制剂--Pralsetinib治疗甲状腺癌,实现生存重磅突破!
2021-06-11 MedSci原创 MedSci原创
Pralsetinib是一种新的、耐受性好的、有效的、每天一次的口服治疗方案,适用于RET改变的甲状腺癌患者。
全球范围内,甲状腺癌的发病率在过去三十年里大幅上升,尤其是在年轻的成年人中,甚至是在青少年中。而甲状腺癌的死亡率却相对稳定在较低的水平,或几乎在所有地方都有所下降。
精准治疗为恶性肿瘤新药、新方法的探索提供了众多方向。其中,RET基因属于比较罕见的致病驱动基因之一,但在甲状腺髓样癌中它却是"万恶之源"。约60%的甲状腺髓样癌患者中可检测出RET基因突变,晚期患者RET突变比例则更高达90%。因此,精准靶向抑制RET基因成为治疗甲状腺髓样癌的关键。
Pralsetinib是一种口服(每日一次)、高效和高选择性的靶向RET变异的在研药物。临床前研究结果显示,pralsetinib对RET融合、RET激活突变敏感,相比VEGFR2, pralsetinib对RET的选择性有90倍提高,并且与已批准的多激酶抑制剂相比也有显著提高。
那么作为RET突变特异性抑制的pralsetinib疗效如何呢?为了探讨上述问题,来自美国德克萨斯大学安德森癌症中心的专家开展了相关研究,结果发表在最新的《柳叶刀》子刊Lancet Diabetes Endocrinology杂志上。
该研究旨在评估pralsetinib在RET突变甲状腺癌患者中的安全性和抗肿瘤活性。ARROW是一项在13个国家的社区和医院的71个地点进行的1/2期开放标签研究,招募了18岁以上的RET改变的局部晚期或转移性实体瘤患者,包括RET突变的髓样甲状腺和RET融合阳性甲状腺癌,同时东部合作肿瘤学组表现状态为0-2。
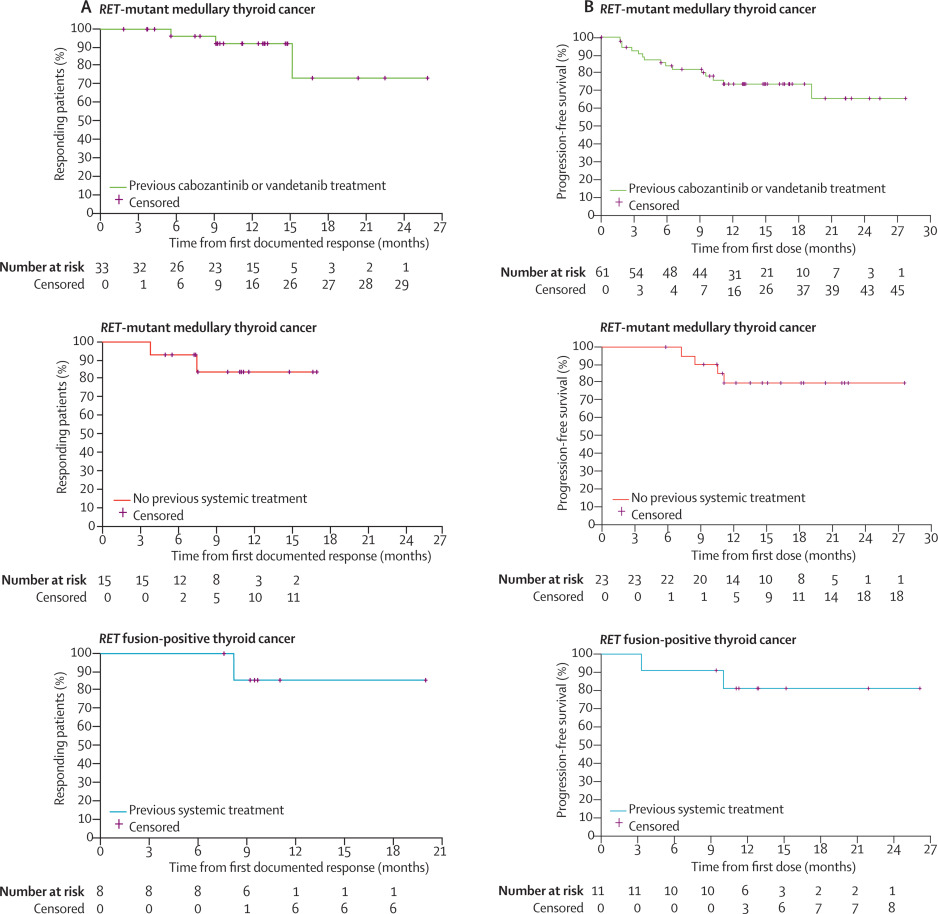
对接受每天一次400mg口服pralsetinib的患者进行评估,直到疾病进展、不耐受、撤销同意或研究者决定为止,其第二阶段主要终点是总反应率和安全性。评估RET突变型髓样甲状腺癌患者的肿瘤反应,这些患者以前接受过卡博赞替尼和/或凡德他尼,或不符合标准治疗的条件,以及以前接受过RET融合阳性甲状腺癌治疗的患者;评估所有RET改变型甲状腺癌患者的安全性。
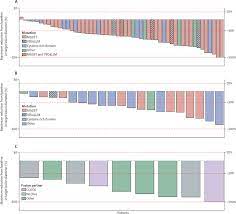
在2017.03.17-2020.05.22期间,有122名RET突变型髓系甲状腺癌患者和20名RET融合阳性甲状腺癌患者入组。在2019.07.11之前接受pralsetinib治疗的基线可测量疾病患者中,治疗无效的RET突变型髓样甲状腺癌患者的总反应率为15/21(71%)(95%CI 48-89),之前接受过卡博赞替尼和/或凡德他尼治疗的患者为33/55(60%)(95%CI 46-73),RET融合阳性甲状腺癌患者为8/9(89%)(95% CI 52-100)。
在2020.05.22前入组的RET融合型甲状腺癌患者中,常见的(≥10%)3级及以上治疗相关不良事件为高血压(24 [17%])、中性粒细胞减少(19[13%])、淋巴细胞减少(17[12%])和贫血(14[10%])。21名患者(15%)报告了严重的治疗相关不良事件,其中最常见的(≥2%)是肺炎(5[4%])。
综上,Pralsetinib是一种新的、耐受性好的、有效的、每天一次的口服治疗方案,适用于RET改变的甲状腺癌患者。
参考文献:
Pralsetinib for patients with advanced or metastatic RET-altered thyroid cancer (ARROW): a multi-cohort, open-label, registrational, phase 1/2 study. https://doi.org/10.1016/S2213-8587(21)00120-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Lancet#
75 举报
#RET#
103 举报
#抑制剂#
83 举报
为甲状腺癌的治疗拓展了更宽阔的渠道
101 举报
#重磅#
68 举报
#RET抑制剂#
75 举报
顶刊就是不一样,质量很高,内容精彩!学到很多
99 举报