Movement disorders:有意思:"菊花"括约肌的肌电图,可辅助鉴别多系统萎缩
2022-02-19 Freeman MedSci原创
EAS肌电图模式的严重程度与MSA的诊断准确性和生存率相一致
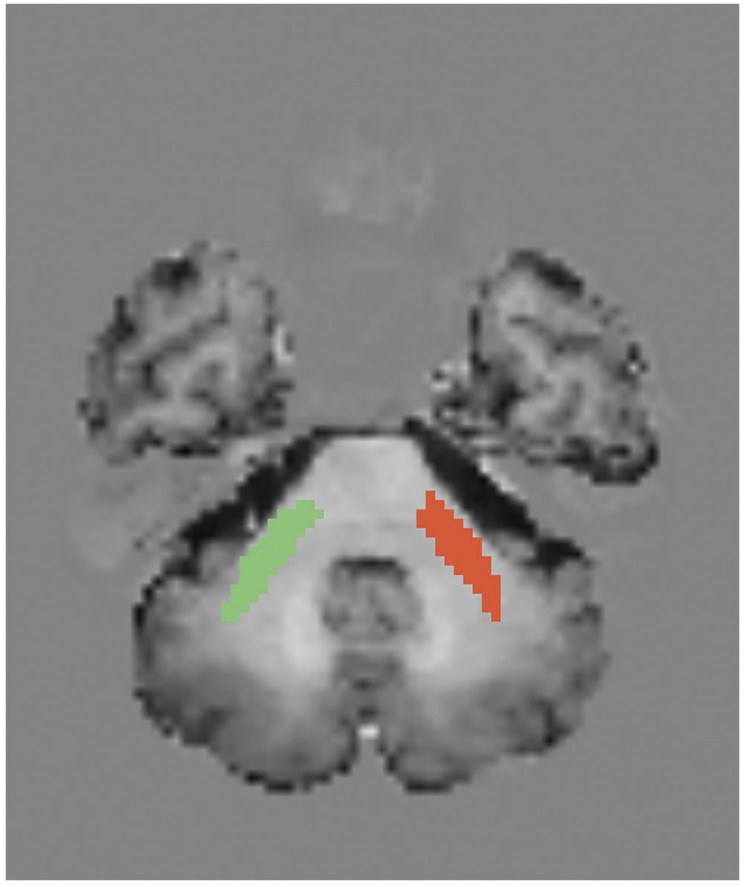
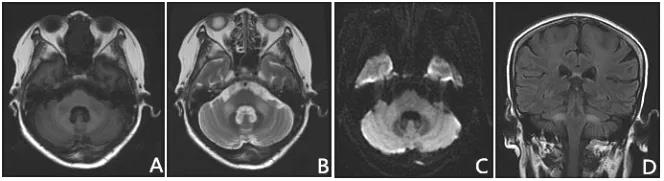
多系统萎缩(MSA)是一种散发性的神经退行性疾病,其特点是自主神经衰弱和帕金森或小脑综合征。早期出现的严重自主神经症状会降低生活质量,并与MSA的不良预后有关。因此,及时诊断对于防止潜在的危及生命的并发症至关重要。然而,MSA的临床表现有时与帕金森病(PD)的现象学相重叠,尤其是MSA患者在早期阶段表现为左旋多巴反应性帕金森病而无明显的小脑受累。有证据表明,帕金森病患者也可表现出自主神经症状,这使诊断情况进一步复杂化。
一些作者建议,肛门外括约肌(EAS)的肌电图(EMG)可能有助于鉴别诊断,特别是在症状发生的头5年内。事实上,与PD患者的正常发现相反,大多数MSA患者表现出EAS的神经源性异常,被认为是Onuf核变性的电生理相关因素,这是MSA的病理特征。尽管有人建议将EAS肌电图纳入MSA的诊断工作中,但一些作者质疑其诊断价值,目前的诊断标准也不承认这项调查是工具箱的一部分。
藉此,意大利的Massimiliano Todisco等人,确定了四种EAS肌电图模式,旨在探索它们在MSA和PD之间的鉴别诊断中的作用,它们与临床特征的关系,以及它们作为MSA预后预测因素的作用。
他们收集了72名MSA患者和21名PD患者的临床数据和EAS肌电图结果。
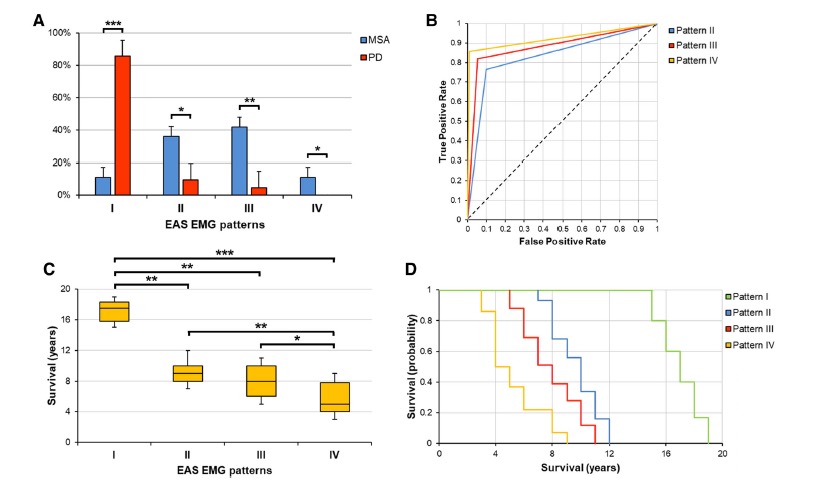
结果。我们确定了四种EAS模式。正常模式在PD中经常被观察到,当在MSA中发现时与生存期延长有关。异常模式在MSA中占主导地位。
最严重的模式与MSA诊断的最高可能性有关,并与MSA队列中最差的预后有关。有EAS异常的MSA患者常常表现为泌尿生殖器症状和大便失禁。
该研究的重要意义在于发现了:EAS肌电图模式的严重程度与MSA的诊断准确性和生存率相一致,并与膀胱和肠道症状的发生率相关。
原文出处:
Todisco M, Cosentino G, Scardina S, et al. Diagnostic and Prognostic Value of External Anal Sphincter EMG Patterns in Multiple System Atrophy. Movement Disorders. Published online 2022:6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#disorder#
85
#disorders#
110
#Disord#
83
#Dis#
93
#ERS#
87
#萎缩#
84
#多系统萎缩#
119
#肌电图#
87