Circulation:心力衰竭和心房颤动患者中控制节奏重要还是与速率控制重要?
2022-03-29 网络 网络
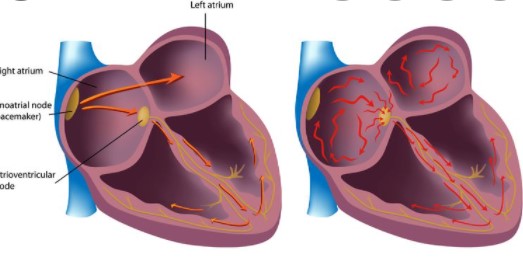
房颤消融是一种治疗始于心脏上腔(心房)的心跳不规律(心律不齐)的手术。
房颤消融是一种治疗始于心脏上腔(心房)的心跳不规律(心律不齐)的手术。这是心脏消融术的一种,通过给心脏上的组织留下疤痕或造成损坏来破坏导致心律失常的错误电信号。如果用于控制心律不齐的药物或其他干预措施无效,可以采用房颤消融。
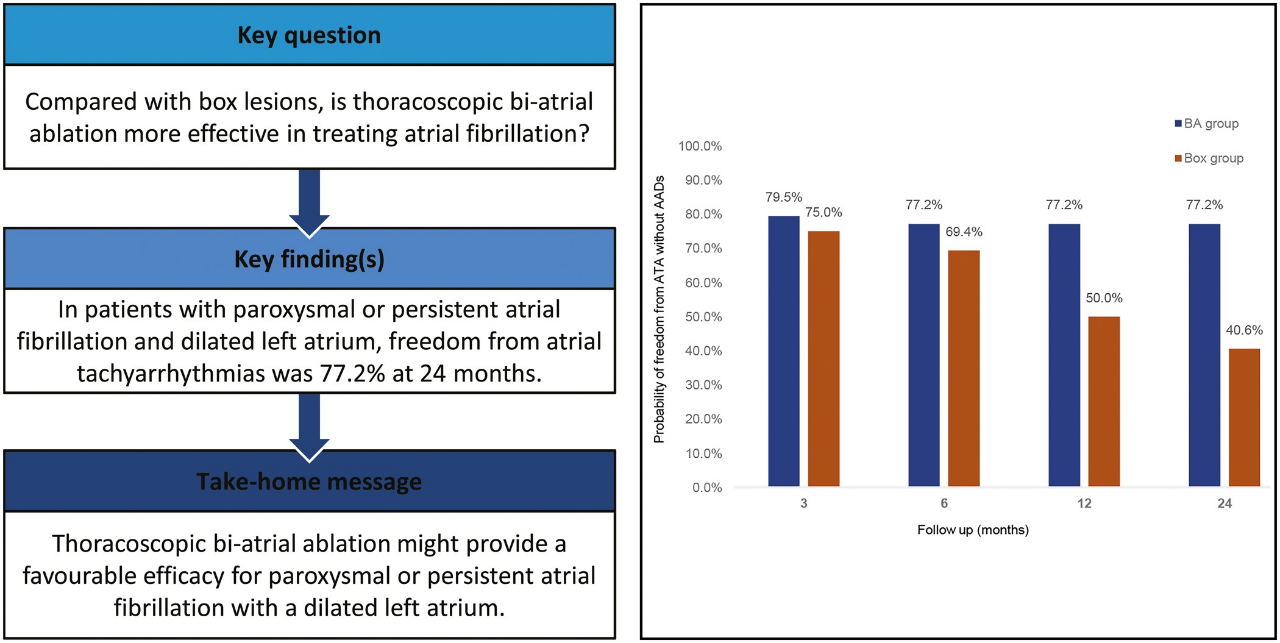
心房颤动(AF)和心力衰竭(HF)经常并存,治疗起来具有挑战性。基于药物的房颤节律控制还没有被证明优于速率控制。将基于消融的节律控制与速率控制进行比较,以评估HF和房颤患者的临床结果是否可以得到改善,结果发表在Circulation杂志上。

这是一项多中心、开放标签的试验,使用中央裁决委员会进行盲法结果评估。高负担的阵发性(6个月内>4次发作)或持续性(持续时间<3年)房颤、纽约心脏协会(NYHA)II-III级HF和NT-proBNP升高的患者被随机分配到基于消融的节奏控制或速率控制。主要结果是全因死亡和所有HF事件的综合,至少随访两年。次要结果包括左心室射血分数(LVEF)、六分钟步行测试和NT-proBNP。
从2011年12月1日至2018年1月20日,411名患者被随机分配到基于消融的节奏控制(n=214)或速率控制(n=197)。主要结果发生在基于消融的节奏控制组的50名(23.4%)患者和速率控制组的64名(32.5%)患者身上。总的来说,节奏控制组主要结局事件风险降低29%(HR=0.71,95% CI(0.49,1.03),P=0.066)。
同时,消融组的LVEF增加(10.1±1.2% vs 3.8±1.2%,p=0.017);六分钟步行距离改善(44.9±9.1米 27.5±9.7米,p=0.025),NT-proBNP显示下降(平均变化-77.1% vs -39.2%,p<0.0001)。MLHFQ在基于消融的心律控制组有更大的改善(LSMD为-5.4,95%CI(-10.5,-0.3),p=0.0036),AFEQT评分也是如此(LSMD为6.2,95%CI(1.7,10.7),p=0.0005)。

综上,在高负荷房颤和HF患者中,基于消融的节律控制与速率控制在全因死亡率或HF事件方面没有统计学差异,然而,基于消融的节律控制比速率控制的结果有改善的非显著趋势。
参考文献:
Randomized Ablation-Based Rhythm-Control Versus Rate-Control Trial in Patients with Heart Failure and Atrial Fibrillation: Results from the RAFT-AF trial. https://doi.org/10.1161/CIRCULATIONAHA.121.057095. Circulation. 2022;0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#速率控制#
108 举报
谢谢分享
99 举报
👍👍👍
103 举报
#心房#
106 举报