Neurology:Andexanet Alfa在凝血因子Xa抑制剂相关性脑出血中的临床意义
2021-10-15 Naomii 网络
近日,有研究人员纳入了在使用FXa抑制剂的情况下出现严重出血的患者,并测量其应用andexanet alfa治疗后止血率和抗Xa活性的变化。
抗凝治疗是脑出血(ICH)的主要危险因素,与较高的死亡率和较差的预后相关。因此,抗凝相关的脑出血早期治疗的关键在于快速逆转抗凝,目的是降低血肿扩大风险。在华法林相关脑出血的治疗中,早期纠正升高的国际标准化比值(INR)水平与降低血肿扩大率、改善临床结果相关。然而, 因子Xa(FXa)抑制剂阿哌沙班和利伐沙班的逆转并不那么简单。
当前指南讨论了凝血酶原复合物浓缩物(PCC)的给药,该浓缩物替代耗尽的凝血因子,而不是直接逆转FXa抑制剂,但其临床疗效存在相互矛盾的证据。最近,一种名为andexanet alfa的新生物诱饵(Andexxa,Portola PharmPharmticals,San Francisco,CA)已根据ANNEXA-4的结果被批准用于急性逆转FXA抑制剂。
近日,有研究人员纳入了在使用FXa抑制剂的情况下出现严重出血的患者,并测量其应用andexanet alfa治疗后止血率和抗Xa活性的变化。ANNEXA-4受其开放标签单臂研究设计的限制,其报告的主要临床结果是止血效果,而不是更以患者为导向的相关结果。andexanet alfa对长期结果的影响尚不清楚,但其成本对许多中心来说可能是令人望而却步的。因此,该研究通过一系列模拟止血效果来确定在FXa抑制剂相关ICH中使用andexanet alfa的潜在临床意义和治疗成本。
研究人员使用单个中心的数据模拟了andexanet alfa在一系列可能的止血作用中的潜在下游影响,该中心用凝血酶原复合物浓缩物(PCC)治疗FXa抑制剂相关ICH,通过多变量回归模型确定FXa抑制剂和非FXa抑制剂患者止血不充分的基线概率,然后使用包括已建立的预测因子和每位患者计算的止血不充分概率的模型确定3个月不良结局的概率(改良Rankin量表)。应用该衍生队列的模型参数自举法来模拟一系列止血改善和相应的结果,然后计算绝对风险降低(相对于PCC)和预防不良结果所需的预计治疗次数(NNT)。
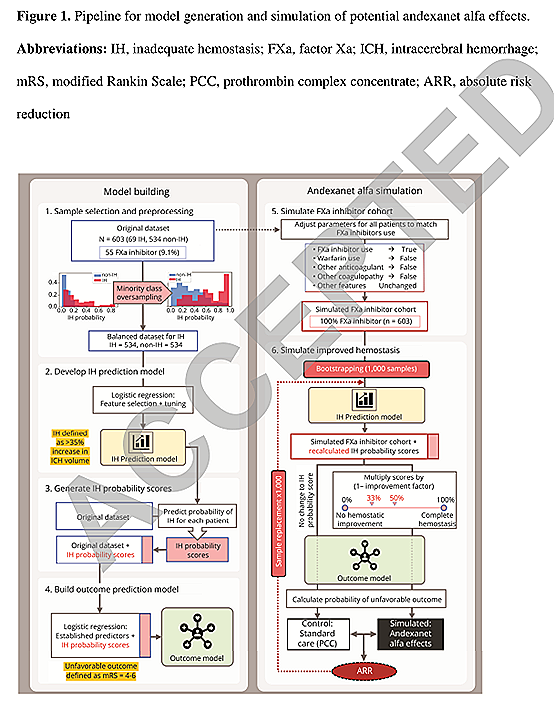
- 使用真实世界患者(总共n=603名;55名FXai)的训练模型在预测止血不充分(AUC 0.78)和不良结局(AUC 0.78)方面具有良好的准确性。止血不充分与不良结局密切相关(OR 4.5,95%可信区间2.0-9.9),发生率为11.4%的FXai患者。
- 在与ANNEXA-4研究类似的模拟FXAI患者中,当止血不充分的概率降低33%时,不良结局的预测绝对风险降低为4.9%(95%CI 1.3%-7.8%),当止血不足的概率降低50%时,预测的不良结局的绝对风险降低为7.4%(95%CI 2.0%-11.9%),预测的NNT分别为21例(累积成本为519,750美元)和14例(346,500美元)。
即使是乐观的模拟止血效果也表明,应仔细考虑andexanet alfa的成本和潜在效益。在确定推荐使用之前,需要进行安慰剂对照随机试验。
文献来源:https://n.neurology.org/content/early/2021/09/21/WNL.0000000000012856.long
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NET#
94
#Xa抑制剂#
82
#andexanet#
100
#ALF#
96
#相关性#
104
#DEXA#
78
#抑制剂#
76
#Neurol#
78
#凝血因子#
117
学习了
130