JNNP:肌萎缩侧索硬化症胸椎型变异的分型
2021-10-22 MedSci原创 MedSci原创
胸椎管变异型肌萎缩侧索硬化症(T-ALS)是一种罕见的亚型,仅影响3%的肌萎缩侧索硬化症(ALS)患者。为了更好地理解这种变异,旨在描述T-ALS的典型特征,包括临床表现、分布模式和预后。
胸椎管变异型肌萎缩侧索硬化症(T-ALS)是一种罕见的亚型,仅影响3%的肌萎缩侧索硬化症(ALS)患者。为了更好地理解这种变异,本文旨在描述T-ALS的典型特征,包括临床表现、分布模式和预后。

对59例T-ALS患者进行了回顾性图表分析,这些患者来自于2002年至2018年间乌尔姆大学医院(德国乌尔姆)神经内科的3549例ALS患者的临床数据库,包括2020年的死亡记录查询。纳入标准为根据经修订的El Escorial标准诊断为明确的ALS,胸肌无力为ALS的首发症状。对照组包括517名非胸椎型肌萎缩侧索硬化症(NT-ALS)患者,来自2010年至2018年间ALS登记处Swabia2的流行病学数据库,不包括原发性侧索硬化症以及家族/遗传形式。本文发表在《神经病学,神经外科学和精神病学杂志》上()

比较了两个队列的临床参数,包括性别、发病年龄、诊断延迟、生存期(从症状开始到死亡的时间)、体重、使用无创通气(NIV)和有创通气(IV)以及传播模式。发病定义为首次轻瘫的发生。对于临床参数的描述,酌情使用绝对和相对频率或中位数和IQR。分类变量比较采用皮尔逊χ2检验。对于连续参数,采用Mann-Whitney U检验。生存率采用Kaplan-Meier法和对数秩检验进行分析。所有统计检验均在α=0.05的双侧显著性水平下进行。
2002年至2018年间,在乌尔姆大学医院(德国乌尔姆)神经内科治疗的3549例ALS患者中,59例(1.7%)患有T-ALS。与NT-ALS相比,T-ALS中的男性占比大(T-ALS:79.7%vs-NT-ALS:55.3%,p<0.001),与NT-ALS中的1.2:1.0相比,T-ALS中的男性:女性比例为3.9:1.0。T-ALS患者的中位发病年龄为65.4岁(IQR 58.7-71.2),T-ALS患者的中位发病年龄为67.8岁(IQR 58.2-74.4)(p=0.08)。在女性患者中,T-ALS的发病年龄比NT-ALS的年轻(T-ALS:60.5岁(IQR 48.8-65.3),而NT-ALS:69.1岁(IQR 59.2-74.7),p=0.004)。
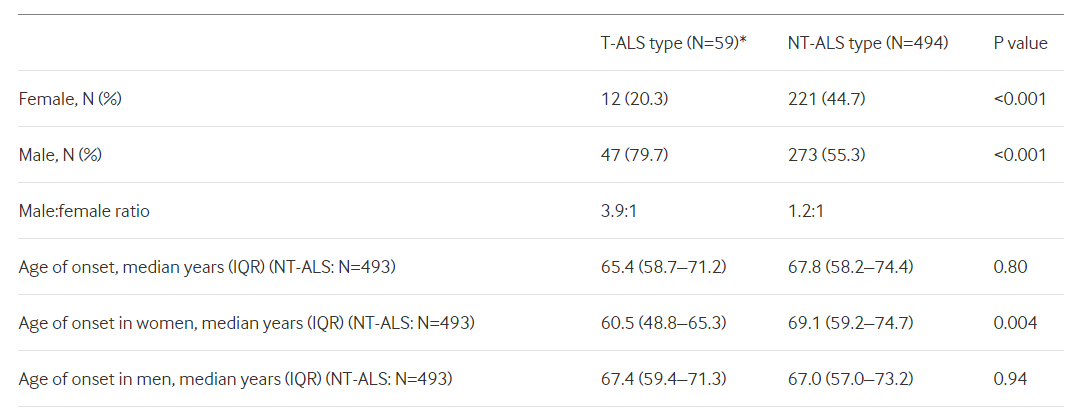
临床结果统计
根据临床表现,我们确定了两个不同的T-ALS亚组,其特征为呼吸肌(n=37)或椎旁肌(n=22)变异。与NT-ALS相比,T-ALS的中位诊断延迟更长(11个月(IQR 6-18)与6个月(IQR 3-11),p<0.001)。T-ALS患者的中位生存期为34个月(95%) CI 28.5至29.5),而25个月(95% NT-ALS(在线补充图1)中的CI 23.0至27.0,p=0.01)。在T-ALS队列中,观察到呼吸性发作和椎旁发作患者之间没有差异(呼吸性发作:中位生存期30个月,95% CI 17.0至42.1;椎旁病变:35.0,95% CI 28.8至41.2;p=0.60)。在T-ALS患者中,60.0%的患者在发病后12个月内开始NIV或IV治疗,而NT-ALS患者仅为7.2%(p<0.001)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#硬化症#
131 举报
#萎缩#
122 举报
#变异#
90 举报
#胸椎#
128 举报
#肌萎缩#
101 举报
#肌萎缩侧索硬化#
130 举报
谢谢分享
125 举报
好文章,谢谢分享。
152 举报