JCO:阿贝西利联合氟维司群对PIK3CA突变HR+/HER2-晚期乳腺癌患者效果良好
2021-03-31 宁咸襄 MedSci原创
近日,JCO在线发表了一项III期SOLAR-1临床试验的患者报告结局。结果显示携带PIK3CA突变的激素受体阳性、人表皮生长因子受体2阴性、晚期乳腺癌患者接受阿贝西利+氟维司群联合治疗,耐受性良好。

近日,JCO在线发表了一项III期SOLAR-1临床试验的患者报告结局。结果显示,携带PIK3CA突变的激素受体(HR)阳性、人表皮生长因子受体2(HER2)阴性、晚期乳腺癌患者接受阿贝西利+氟维司群联合治疗,耐受性良好。

图1 论文封面截图
在美国,HR+、HER2-亚型乳腺癌占乳腺癌病例的70%以上。患者的HR +推荐的标准护理用于初始治疗,HER2-晚期乳腺癌(ABC)是依次使用的基于内分泌疗法(ET)的多条线。这种方法的合理性在于,在转向化疗之前,必须尽可能长时间维持ABC患者的生活质量(QoL)。三类靶向疗法(雷帕霉素抑制剂,CDK4/6抑制剂和PI3K抑制剂的哺乳动物靶点)与ET结合使用可改善无进展生存期(PFS),因此可延迟化疗。这三类靶向疗法现在被认为是护理标准。多项研究一致表明,CDK4/6抑制剂可维持ABC患者的QoL。然而,目前还没有PI3K抑制剂治疗的患者的生活质量数据报告。磷脂酰肌醇-4,5-二磷酸肌醇3-激酶催化亚基α(突变PIK3CA)基因在患有HR+、HER2-乳腺癌的患者中约有40%,并与不良预后的患者ABC相关联。
III期SOLAR-1临床试验的PIK3CA突变队列纳入了341位受试者,1:1随机接受阿贝西利 300mg+氟维司群 500mg或安慰剂+氟维司群 500mg治疗,在第一疗程的第1天和第15天及后续28天疗程的第1天给药。受试者运用欧洲癌症研究与治疗组织生命质量测定量表 (EORTC QLQ-C30 V3.0 )和简明疼痛评估表(BPI)进行自评。 结果显示,两组的总体健康状况/生活质量(QoL)和功能状况均维持在基线水平(平均变化<10分),且两组总体疗效在总体健康状况/QoL评分方面出现10%恶化的时间类似(HR 1.03),评分没有显著差异(p=0.101)。
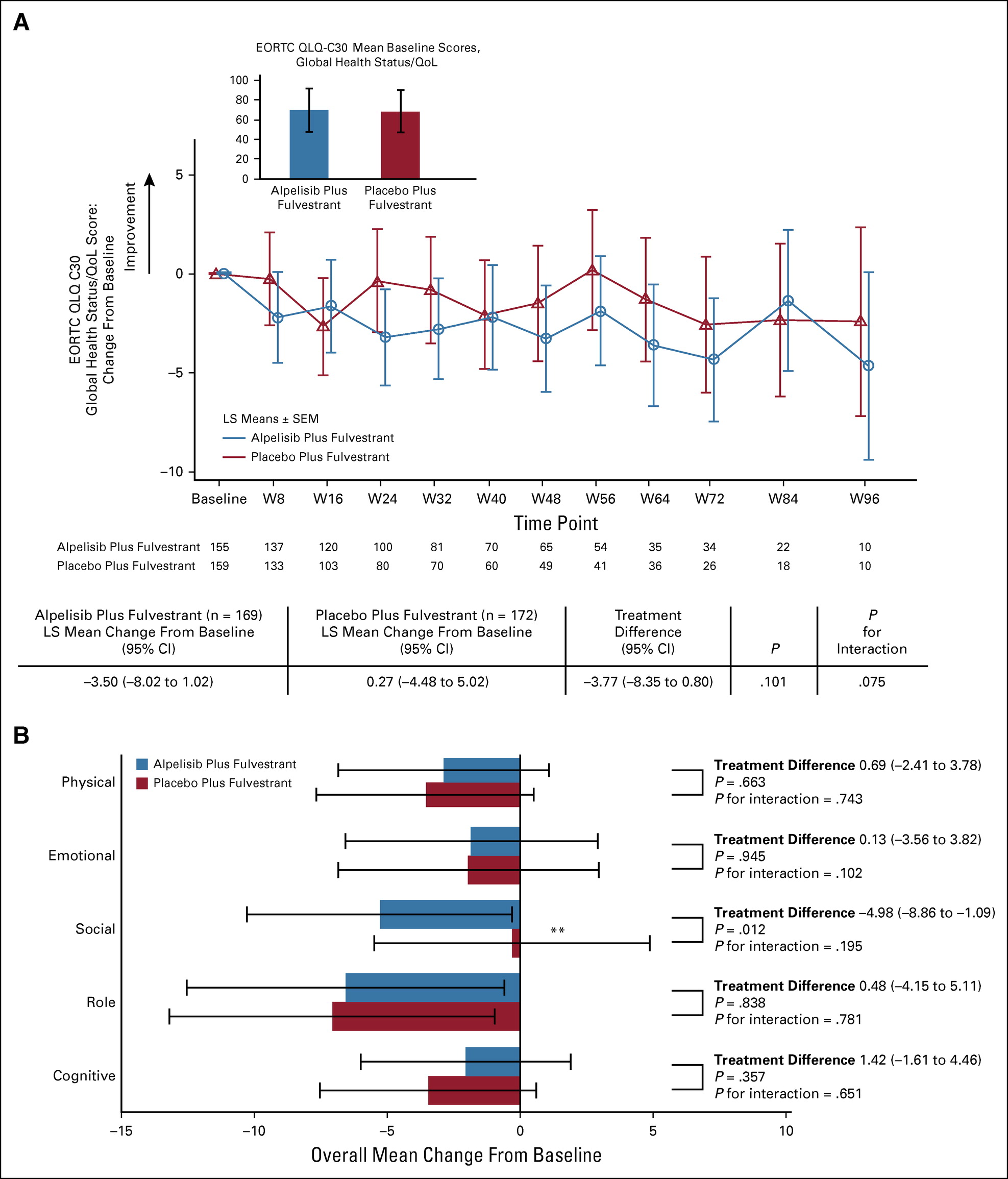
图2 EORTC QLQ-C30全球健康状况/QoL量表评分相对于基线的变化
不过,与安慰剂组相比,阿贝西利组的社会功能、腹泻、食欲减退、恶心或呕吐及疲劳的症状分量表均出现恶化。 虽然阿贝西利组最严重疼痛的评分有改善,但差异不显著(32% vs 42%,第24周,p=0.09)。 在SOLAR-1临床试验中,尽管阿贝西利组出现与阿贝西利治疗相关副作用的症状分量表评分恶化,但两组患者的总体健康状况/QoL评分恶化情况无统计学差异。以往SOLAR-1研究数据就证明了阿贝西利联合氟维司群对于PIK3CA突变HR+/HER2-晚期乳腺癌患者的有效性与耐受性,而该分析进一步支持了该类患者使用阿贝西利治疗的良好耐受性。
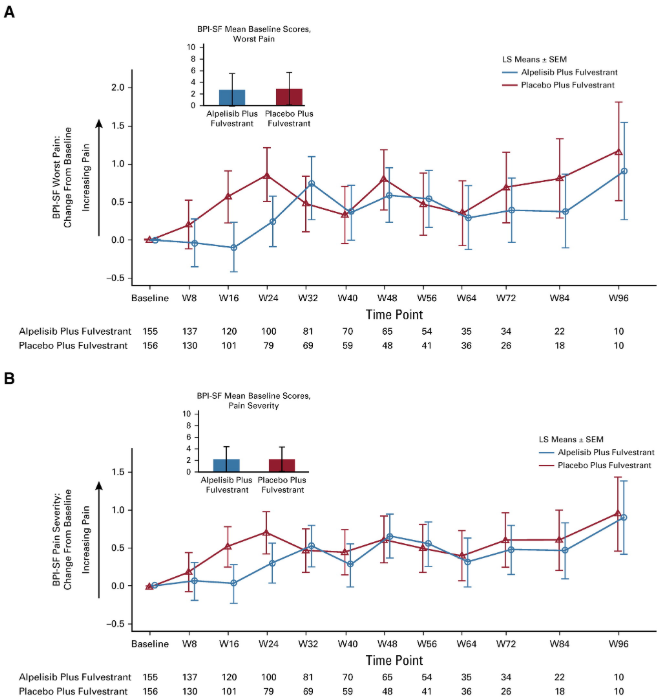
图3 BPI-SF疼痛严重程度指数
参考文献:
Ciruelos EM, Rugo HS, Mayer IA, Levy C, Forget F, Delgado Mingorance JI, Safra T, Masuda N, Park YH, Juric D, Conte P, Campone M, Loibl S, Iwata H, Zhou X, Park J, Ridolfi A, Lorenzo I, André F. Patient-Reported Outcomes in Patients With PIK3CA-Mutated Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer From SOLAR-1. J Clin Oncol. 2021 Mar 29:JCO2001139. doi: 10.1200/JCO.20.01139. Epub ahead of print. PMID: 33780274.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#PIK3CA突变#
115
#PIK3CA#
124
#HER2-#
88
#JCO#
88
怎么才能得到积分了。
145
#乳腺癌患者#
103
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
124
学习了
153