
题目:小细胞肺癌亚型的真实世界多组学特征,揭示临床相关生物标志物的不同表达
Real-world multiomic characterization of small cell lung cancer subtypes to reveal differential expression of clinically relevant biomarkers.
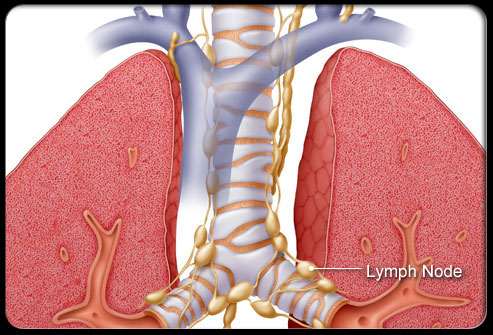
小细胞肺癌(SCLC)是一种神经内分泌肿瘤,在临床上被视为一种预后不良的单一疾病。根据转录因子ASCL1、 NEUROD1、 POU2F3和YAP1四个分子的主要表达特征性地定义了四种SCLC亚型(SCLC-A,SCLC-N,SCLC-Y和SCLC-P)。
近日,有新的证据表明,YAP1的表达与T细胞炎症表型有关,而且SCLC在MYC驱动的NOTCH信号激活的介导下,具有明显的肿瘤内异质性。因此,该研究对真实世界的SCLC患者样本进行了大规模的分析,以检查不同SCLC亚型的临床相关生物标志物的表达。
方法
研究人员使用下一代DNA测序(592个基因组)、RNA测序(整个转录组)和免疫组化法对437个小细胞肺神经内分泌肿瘤(包括7.3%的高级别神经内分泌肺癌)进行了全面的分子分析。
根据四个转录因子的相对表达,将肿瘤分层为5个亚组(SCLC-A/N/Y/P和-混合组)。对各亚组的关键基因和先前验证的免疫特征(T细胞发炎、NK细胞和STING途径特征)的RNA表达进行了评估。通过Chi-square、Fisher's exact test或Mann-Whitney U test检验其显著性。
结果
研究队列的中位年龄为66岁(IQR:59-72),50.6%的患者为女性。大多数(67.3%)的样本来自于转移部位。按表达方式对肿瘤进行分层,结果是35.7%的SCLC-A、17.6%的SCLC-N、21.1%的SCLC-Y、6.4%的SCLC-P和19.2%的SCLC混合样本。
与转移部位的肿瘤相比,YAP1的表达在原发肿瘤中明显增加(P < 0.001)。在从中枢神经系统获得的14个肿瘤中,SCLC-N(36%,n = 5)是最常见的亚型。dMMR/MSI-高(MMR蛋白阴性表达/每个肿瘤≥46个改变的位点)总体上是罕见的(0.5%,n = 2);TMB(中位数为9-10个突变/Mb)在SCLC亚型之间类似。
SCLC-Y与T细胞炎症、NK细胞和STING通路特征的最高表达有关(各P < 0.0001)。MYC和NOTCH基因表达(NOTCH1/2/3/4)与YAP1表达密切相关。
共同突变的分析显示,EGFR敏感突变(L858R和19号外显子缺失)在SCLC-N肿瘤中反复出现(5.2%,n = 4)。SNF11、SSTR2和MYC的表达在SCLC亚型中差异显著(各P<0.001),在SCLC-N中观察到SNF11和SSTR2的最高中位表达,而MYC表达在SCLC-P中最高。
结论
该研究分析代表了通过全转录组测序分析人类SCLC肿瘤的最大现实世界数据集。不同SCLC亚型的免疫基因和预测性生物标志物的差异性表达可能为SCLC的合理和个性化治疗方法提供治疗漏洞。
题目:AMG 757是一种半衰期延长的双特异性T细胞吞噬剂(BiTE)免疫肿瘤疗法,用于治疗小细胞肺癌(SCLC)的最新结果
Updated results from a phase 1 study of AMG 757, a half-life extended bispecific T-cell engager (BiTE) immuno-oncology therapy against delta-like ligand 3 (DLL3), in small cell lung cancer (SCLC).
小细胞肺癌(SCLC)是一种侵袭性的神经内分泌肿瘤,容易发生早期转移,占所有肺癌的10%-15%,与5年生存率较低。在对以依托泊苷和铂类为基础的化疗有或无放疗的初步反应后,疾病复发和抗治疗很常见。尽管反应率相对不高,但免疫检查点阻断疗法增加了SCLC的总生存率(OS)。
现阶段,美国加速批准anti-PD-1抗体nivolumab和pembrolizumab用于治疗以铂类为基础的化疗和至少一种其他治疗方法的进展的转移性SCLC;然而,随后的研究并没有证实OS增加。靶向治疗的前景在SCLC中也尚未实现;一种DLL3靶向的抗体-药物结合物有早期临床活性的证据,在随后的III期试验中没有显示出益处。SCLC患者仍然迫切需要具有不同作用机制的治疗药物。
双特异性T细胞吞噬剂(BiTE)分子是一种经过临床验证的治疗方式,可将患者的T细胞重定向到杀死肿瘤细胞。AMG 757是一种半衰期延长的BiTE免疫肿瘤疗法,与肿瘤细胞上的DLL3和T细胞上的CD3结合,导致T细胞依赖性地杀伤肿瘤。
本次研究报告了AMG 757在SCLC中正在进行的1期研究中10个队列的最新安全性、疗效和药代动力学数据。
方法
每2周静脉注射AMG 757(0.003-100mg)±阶梯式给药。符合条件的患者(pts)在接受了≥1个以铂类为基础的治疗方案后,SCLC出现进展。抗肿瘤活性由改良的RECIST 1.1评估。
结果
截至2021年1月11日,有64名患者在10个剂量水平(DLs; 0.003-100 mg)下接受了≥1个AMG 757剂量,并可用于分析。中位年龄为64(范围,32-80)岁;63名患者(98%)的ECOG PS为0-1,先前治疗线的中位数为2(范围,1-6),其中28名患者(44%)先前接受PD-1/PD-L1治疗。中位治疗时间为6(范围为0.1-71)wk。53名患者(83%)出现了治疗相关的AE:16名(25%)≥3级(G),4名(6%)≥G4,1名(2%)G5(肺炎;DL5[0.3mg])。AEs导致1名患者停药(G3级脑病,DL10[100mg])。27名患者(42%)报告了细胞因子释放综合征(CRS;根据Lee 2014标准进行分级)。7人(11%)为G2,1人(2%)≥G3。CRS主要表现为发热(31%)、心动过速(17%)、恶心(13%)、疲劳(9%)和低血压(9%)。CRS通常是可逆的,并通过支持性护理、皮质类固醇和/或抗IL-6R来处理。CRS并没有导致任何治疗的中断。
在接受10个DL治疗的60名患者中,随访时间中位数为4.2(范围为0.2-18.6)月,对疗效进行评估。8/60名患者(13%)在所有DL中被确认为PR,其中5/8名患者(63%)在100mg(DL10)时获得未确认的PR。反应的中位时间为1.7(范围为1.2-3.7)月。71%的患者(95%CI:26,92)的估计反应持续时间大于6个月,有任何PR。疾病控制率为43%,23/60例患者(38%)出现了肿瘤缩小。在评估的剂量范围内,AMG 757的血清暴露量大约按剂量比例增加。
结论
剂量达100mg时,AMG 757的安全状况可以接受。反应是快速和持久的。在不同的剂量范围内都有令人鼓舞的抗肿瘤活性,在最高剂量下有5/8名患者(63%)正在进行未经确认的PR。该研究正在进行中;将提交最新数据,包括反应率和反应持续时间。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASC#
97
学习了
116
棒
124
学习
113
#ASCO2021#
153