急性心肌梗死(AMI)所致的心源性休克(CS)是心梗患者主要死亡因素之一,其中主要的发病机制为急性心肌梗死后引起急性左右心衰竭、周围血管阻力改变、重要器官供血不足,引发炎性反应,最终多器官功能衰竭。临床治疗中,早期稳定血流动力学、行血运重建是心源性休克的主要治疗方式。
尽管在血管重建策略和机械循环支持(MCS)设备方面取得了进展,但急性心肌梗死和心源性休克患者的死亡率仍然很高。为了阐明合并下肢外周血管疾病(PAD)与CS和AMI的结果之间的关系,来自哥伦比亚大学欧文医学中心/纽约长老会医院心脏病科的专家开展了相关研究,结果发表在JACC杂志上。
2015年10月1日至2018年6月30日住院的CS和AMI的医疗保险受益人中定义了PAD状态。到2018年12月31日确定的主要结果包括院内和院外的死亡率。次要结果包括出血、截肢、中风和下肢血管再造。对混杂因素进行调整的多变量回归模型被用来估计风险。亚组分析包括接受MCS治疗的患者和接受冠状动脉血运重建的患者。
在71690名患者中,5.9%(N = 4259)有PAD。平均年龄为77.8±7.9岁,58.7%为男性,84.3%为白人。累计院内死亡率为47.2%,总的来说,有PAD的患者死亡风险大50%(56.3% vs 46.6%;调整后的OR=1.50;95% CI:1.40-1.59)。
PAD患者的院内截肢(1.6% vs 0.2%;调整后的OR:7.0;95% CI:5.26-9.37)和院外死亡(67.9% vs 40.7%;调整后的HR:1.78;95% CI:1.67-1.90)的风险也分别高6倍和78%。此外,PAD患者较少使用机械循环辅助(21.5% vs 38.6%),并且与较高的死亡率、下肢血管再造的需要和截肢风险有关。研究结果在接受冠状动脉血运重建的患者中是一致的。
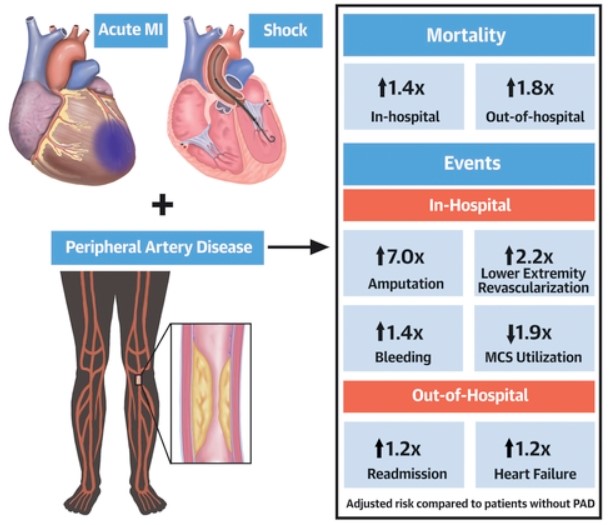
图形摘要总结
综上,在出现AMI和CS的患者中,PAD与较差的肢体结果和生存率有关。除了较低的机械循环辅助使用率外,那些接受MCS的PAD患者的死亡率、下肢血管再造和截肢率都有所增加。
参考文献:
Outcomes Associated With Peripheral Artery Disease in Myocardial Infarction With Cardiogenic Shock. J Am Coll Cardiol. 2022 Apr, 79 (13) 1223–1235
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
92
#ACC#
89
#心源性休克#
136
#外周动脉#
111
#心源性#
107