JNNP:偏瘫型ALS:两名尸检患者的临床病理特征
2021-04-22 MedSci原创 MedSci原创
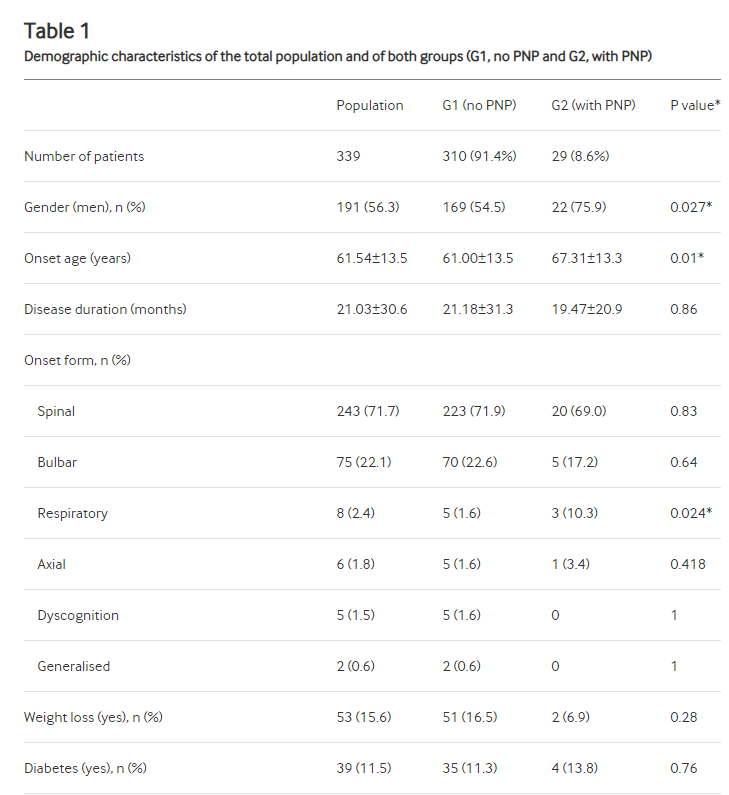
在肌萎缩性侧索硬化症(ALS)中,尚不清楚初始病变如何在上,下运动神经元(UMN和LMN)系统中发展并进一步扩展。使用细胞或动物模型进行的ALS的多项研究表明,与疾病相关的蛋白,与反应相关的DNA结合
在肌萎缩性侧索硬化症(ALS)中,尚不清楚初始病变如何在上,下运动神经元(UMN和LMN)系统中发展并进一步扩展。使用细胞或动物模型进行的ALS的多项研究表明,与疾病相关的蛋白,与反应相关的DNA结合蛋白43 kDa(TDP-43)通过依次的细胞间传递和/或顺行性/逆行轴突运输。但是,通常难以追踪活着患者的疾病进展路线或TDP-43在人体尸体解剖组织中的传播痕迹。部分原因是由于ALS的临床表型多样,以及由此导致的疾病发展速度和方式的个体差异 。
在ALS的各种变体中,偏瘫型ALS的特征是整个疾病的临床症状均显着不对称。 在此,本文报道了两例偏瘫型ALS尸检病例的临床病理特征,其中特别提及了按时间顺序演变之间的临床病理联系。偏侧的临床症状和不对称的病变扩展以及UMN和LMN系统之间的退化联系。本文将进一步讨论可能有助于上述疾病的病理机制。
患者是两名分别在70年代和80年代无关的男性,最初表现为单侧(患者1,左侧;患者2,右侧)腿部无力,并在接下来的3年和2年内分别累及同侧臂和延髓肌。在这两名患者中,包括痉挛和反射亢进在内的UMN体征也出现在肌肉无力的主要一侧。他们在发作后3年和4年死于呼吸衰竭, 肢体无力不对称仍是在线补充方法的明显证据。尸检显示,运动系统的退化程度显然反映了运动症状的临床不对称性和按时间顺序的演变。
在患者1中,LMN病变在左腰脊髓严重(图1A-4),在左颈脊髓中度(图1A-2)和在右腰脐中(图1A-3)是轻度;右颈脊髓未见明显的病变(图1A-1)。此外,左侧的腰椎前根和腰肌的萎缩更为严重(图1B–D)。同时,在运动皮层中,右腿运动区的变性很严重,右手和面部运动区的变性很严重,左腿运动区的变性很轻(图1E)。患者2表现出的运动系统退化。在这两名患者中,TDP-43阳性和pTDP-43阳性的神经元和神经胶质细胞质包涵体(NCI和GCI)形成于少突胶质中,相对局限于运动神经元系统,但在几个非运动区也很明显。在运动皮层中,更严重退化的一侧(患者1,右;患者2,左侧)的腿部和手部运动区域的NCI和GCI均超过同侧面部和对侧腿部运动区域的NCI和GCI。在脊柱前角,GCIs侧向于临床上占优势的一侧,而对于NCI随LMN死亡而消失的NCI则没有这种不对称性。在这两名患者中,舌下核均受到神经元丢失和pTDP-43病理的对称影响。在下肢运动区,严重退化的一侧Iba-1阳性小胶质细胞较多。
患者1的尸检结果
在目前的患者中,LMN和UMN病变侧向同一侧,暗示了UMN和LMN系统之间可能存在退行性联系。此外,组织学检查显示,在控制最初受累的腿部区域,两个运动系统的退化最为严重。此外,在UMN系统中,控制临床上占优势的肢体运动区域中存在大量的pTDP-43积累。病理严重程度与临床进展模式之间的这种牢固相关性,以及UMN和LMN系统变性之间的关联,进一步支持了以下假设:UMN和LMN系统变性在偏瘫型ALS中协同进行。本研究的局限性在于缺乏在疾病晚期的详细肌电图研究,本文目前的发现表明,偏瘫型ALS的发病机制可能促进在相互连接的UMN和LMN系统中的连续病变扩散。有必要进行进一步的研究以生化表征这种异常ALS表型所固有的pTDP-43,在该表型中,在UMN和LMN水平上的连合传播都减弱了。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#病理特征#
132
#临床病理#
130
。
157
#尸检#
127
#偏瘫#
122
学习了,涨知识了!
134