Circulation:重磅!科学家成功将结缔组织细胞重编程为心肌细胞
2016-11-12 佚名 生物谷
图片摘自:timesofindia.indiatimes.com 最近,来自格莱斯顿研究所(Gladstone Institutes)的科学家们通过研究鉴别出了两种化学物质或能改善心脏瘢痕组织转化成为健康心肌组织的能力,相关研究刊登于国际杂志Circulation上,该研究或将帮助研究人员开发新型有效的治疗心力衰竭的疗法。 心力衰竭每年影响着570万美国人的健康,而且每年能够花费国家307

图片摘自:timesofindia.indiatimes.com
最近,来自格莱斯顿研究所(Gladstone Institutes)的科学家们通过研究鉴别出了两种化学物质或能改善心脏瘢痕组织转化成为健康心肌组织的能力,相关研究刊登于国际杂志Circulation上,该研究或将帮助研究人员开发新型有效的治疗心力衰竭的疗法。
心力衰竭每年影响着570万美国人的健康,而且每年能够花费国家307亿美元,最关键的是目前并无疗法治疗心力衰竭;当心肌受损时,机体就无法修复死亡或损伤的细胞,文章中,研究者就深入分析了心脏中细胞的重编程机制,以此来对心肌细胞进行再生,这或许有望治疗并且治愈患者的心力衰竭。
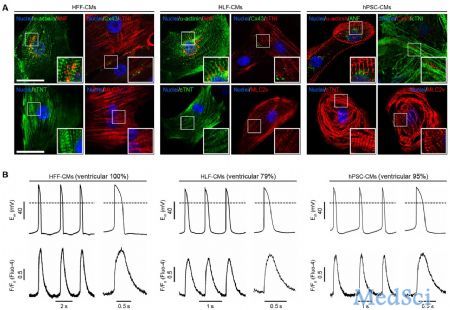
仅需要三种转录因子就能够将小鼠机体的结缔组织细胞重编程为心肌细胞,当心脏病发作后,结缔组织就会在损伤部位形成疤痕组织,从而诱发心力衰竭的发生,这三种转录因子Gata4,Mef2c,Tbx5(GMT因子)能够互相协作开启结缔组织细胞中的基因表达,同时关闭其它不必要基因的表达,最终对损伤的心肌细胞进行有效修复,但这种方法并不简单,而且也仅有10%的细胞能够从疤痕组织细胞转化成为心肌组织细胞。
这项研究中,研究者检测了5500种化合物对改善上述过程的作用,最后他们发现了两种关键的化合物能够将转化的心肌细胞数量增加八倍,此外这两种化合物还能够加速细胞的转化过程,从而在一周内完成需要6-8周的细胞转化工作。医学博士Deepak Srivastava认为,利用GMT因子进行的直接心脏细胞重编程极具潜力,同时也是非常有效的,基于我们前期的筛选工作,如今我们通过研究发现,化学性地抑制两种在胚胎形成过程中处于活性的生物学途径或许就能够加速心肌细胞产生的速度、质量以及数量。
第一种化学物质能够抑制一种生长因子的功能,而这种生长因子能够帮助细胞生长和分裂,而且对于损伤后组织修复非常重要;第二种化学物质能够抑制一种重要的通路,该通路能够调节心脏发育;通过将GMT因子同这两种化学物质进行结合,研究人员就能够成功改善遭受心力衰竭小鼠机体的心肌以及心脏功能。同时研究者还能够利用这些化学物质直接指导人类细胞的心脏重编程,而且这些化合物也能够简化研究者的研究步骤来帮助开发出更好地治疗心力衰竭的疗法。
最后研究者Tamer Mohamed表示,心力衰竭影响着全球很多人的健康,如今我们并没有治疗心力衰竭的有效疗法,如今基于这种直接对心肌细胞的重编程技术,我们或许就有望将药物同基因疗法相结合来开发出治疗心力衰竭的新型靶向性疗法。
原始出处
Tamer M. A. Mohamed, Nicole R. Stone, Emily C. Berry, Ethan Radzinsky, Yu Huang, Karishma Pratt, Yen-Sin Ang, Pengzhi Yu, Haixia Wang, Shibing Tang, Sergey Magnitsky, Sheng Ding, Kathryn N. Ivey and Deepak Srivastava.Chemical Enhancement of In Vitro and In Vivo Direct Cardiac Reprogramming.Circulation.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞重编程#
86
#结缔组织#
78
xuexile
66
#重磅#
0
学习了,赞一下
73
好厉害呀!
89