J Orthop Surg Res:中国学者发文股骨头坏死患者初次全髋关节置换术后1年行走独立性丧失的发生率和风险预测模型
2024-09-24 医路坦克 MedSci原创 发表于上海
全髋关节置换术(THA)治疗股骨头骨坏死(ONFH)患者术后活动能力的评估是有限的。本研究旨在确定原发性THA术后1年ONFH患者丧失行走独立性(LWI)的发生率和危险因素,并建立和验证预测图。
股骨头坏死(Osteonecrosis of femoral head, ONFH)影响了全世界超过2000万人,由于股骨头塌陷率高达85%,通常需要手术治疗。全髋关节置换术(THA)仍然是晚期ONFH最有效和最广泛应用的手术;然而,7.2%的患者术后不能恢复独立行走。丧失行走独立性(LWI)的患者面临高达13%的翻修风险和77%的残疾风险增加,这给医疗保健系统带来了极大的负担。因此,改善接受THA的ONFH患者的行走结果是必要的。
一些研究报告了THA术后的行走效果。Singh等通过问卷对5707例患者进行了评估,发现5.7%的患者术后2年存在严重的行走限制。另一项对753例老年髋部骨折患者的研究显示,36.3%的患者在术后180天发生LWI。然而,现有的步行评估主要集中在髋部骨折或骨关节炎患者,很少有关于ONFH人群的报道。
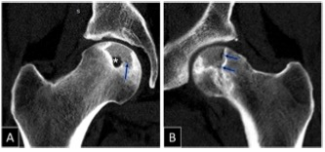
零星发表的文献已经确定了影响术后功能的因素,如Association Research Circulation Osseous (ARCO)分期和腿长差异(LLD),但没有优先考虑独立行走。随着指南强调行走评估的重要性,需要高质量的证据来为ONFH患者接受THA后的行走恢复提供信息。综上所述,本研究通过扩大样本,确定了因ONFH而接受原发性THA的患者术后1年LWI的发生率和临床危险因素,同时建立并验证了预测图。
方法:回顾性分析2014年10月至2018年3月在一家三级转诊医院接受原发性单侧THA治疗的ONFH患者的前瞻性收集数据。功能独立测量-运动量表用于量化行走独立性,并在术后一年的连续随访中记录,将最终得分低于6分的患者分类为LWI。多因素logistic回归分析确定LWI的独立危险因素,并根据分析结果构建预测模态图。使用2018年4月至2019年4月的患者作为外部验证集评估模型的稳定性。
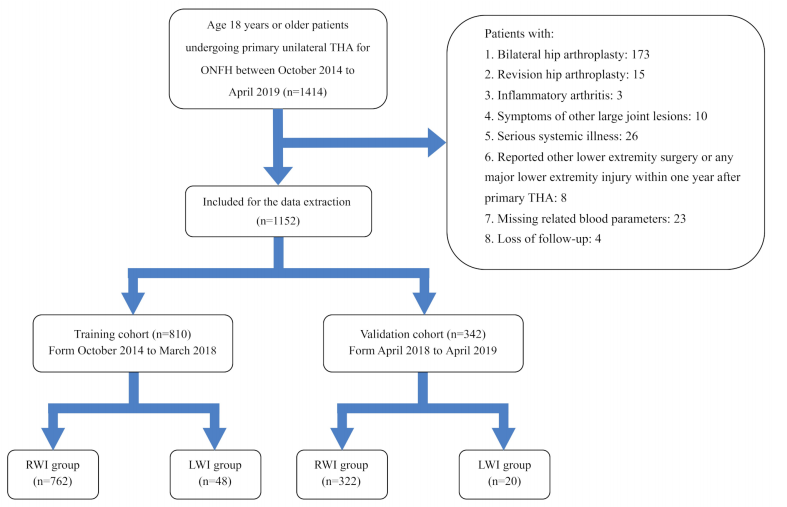
患者选择流程图。THA:全髋关节置换术;ONFH:股骨头骨坏死;RWI:恢复行走独立性;LWI:失去行走的独立性
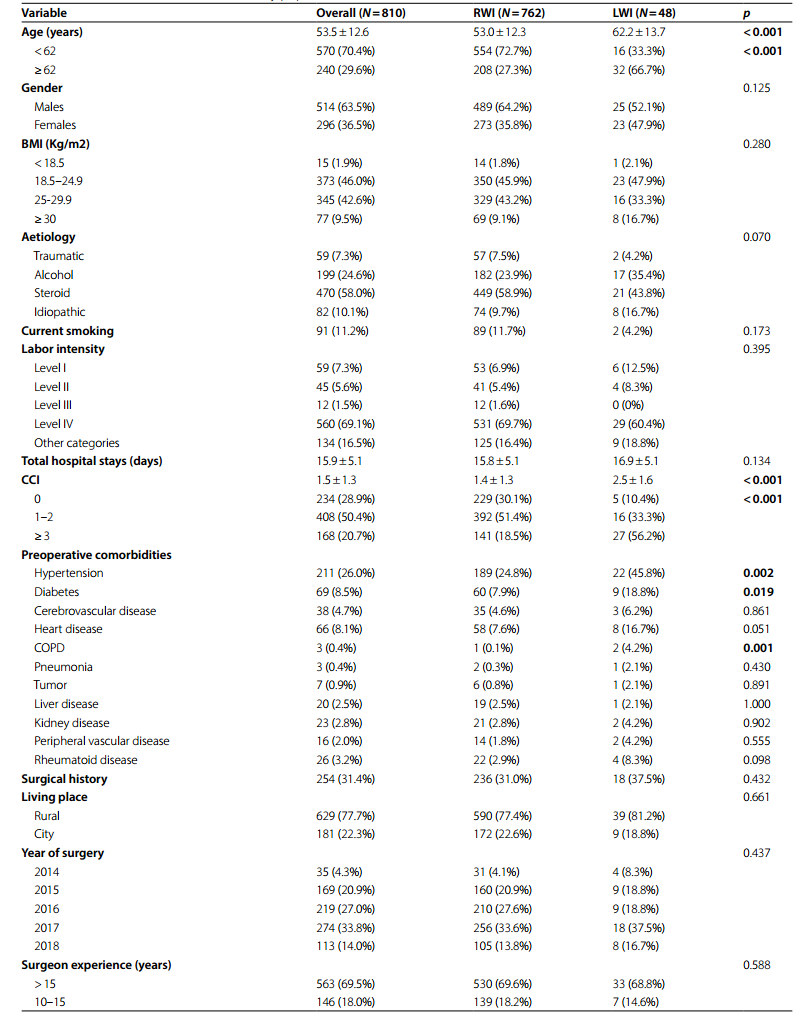
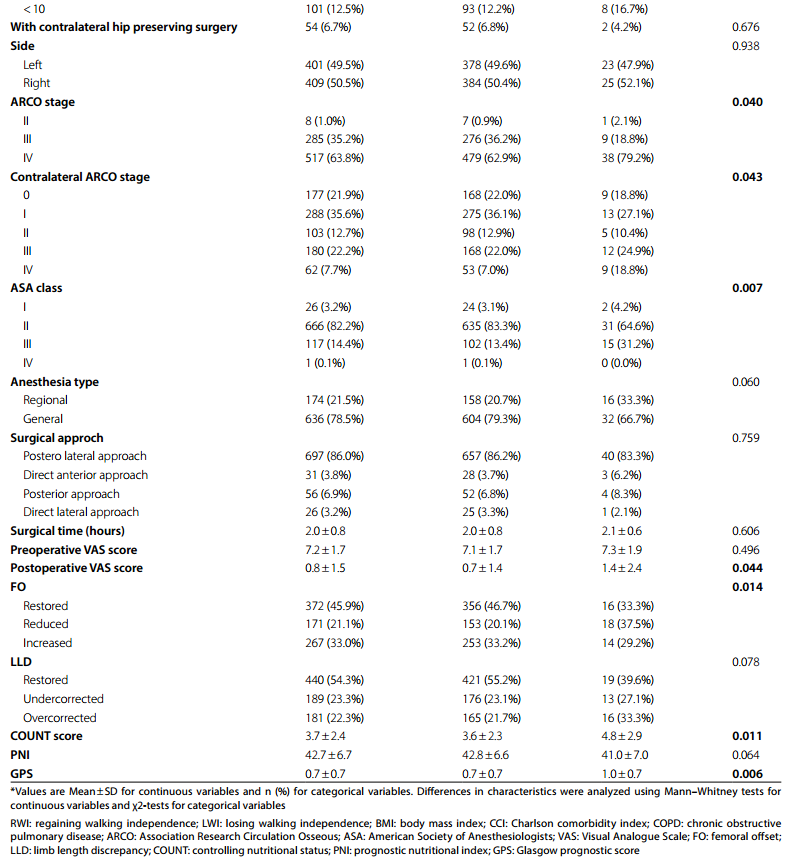
研究人群的基线特征
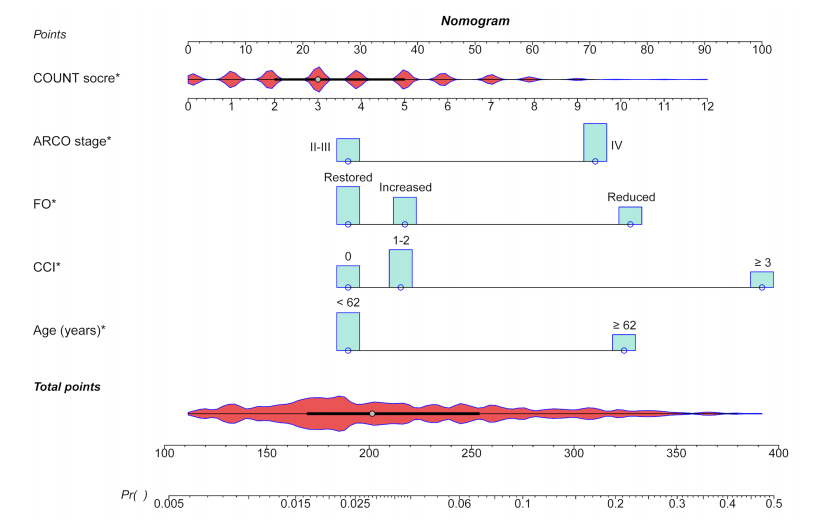
预测ONFH患者术后1年LWI的Nomogram (x线图)。将5个因素计算成LWI预测nomogram,每个预测因子在最上面的点数轴上被赋予一个给定的分数,在最下面的概率轴上显示总点数对应的LWI预测概率。LWI:丧失行走能力;计数:控制营养状况;ARCO:协会研究循环骨;FO:股偏置;查理森共病指数
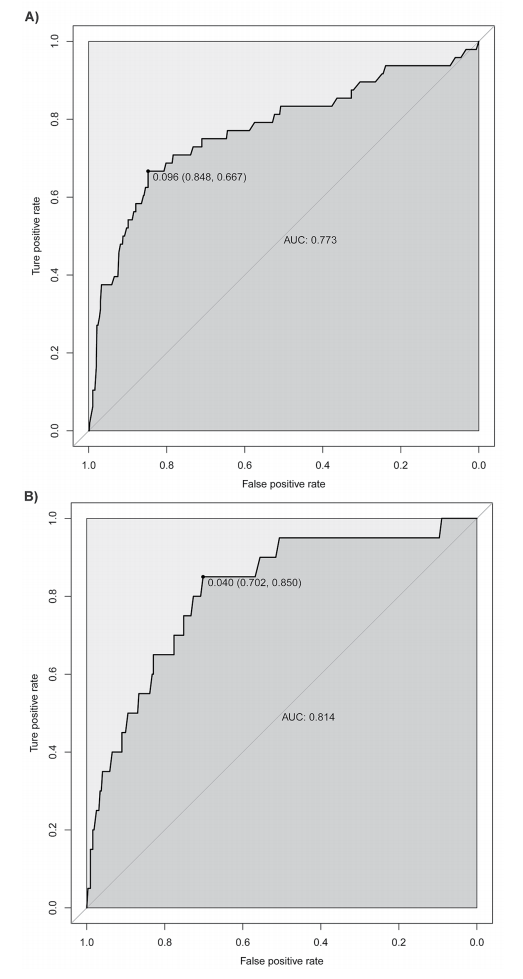
训练集(A)和验证集(B)的nomogram Receiver-operating characteristic (ROC)曲线。nomogram的预测准确度与曲线下面积(AUC)呈正相关。在训练集和验证集上,模态图的AUC分别为0.773和0.814,表明该模型具有较好的判别能力
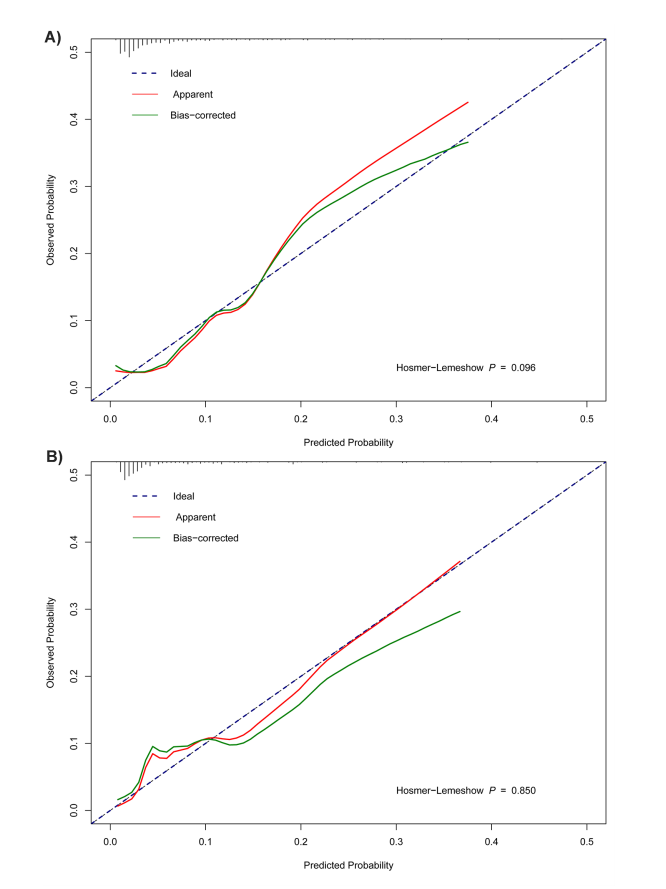
训练集(A, P=0.096)和验证集(B, P=0.850)的nomogram校准曲线。x轴表示模型的预测概率,y轴表示实际概率。红、绿曲线与理想虚线越接近,模态图的预测一致性越好
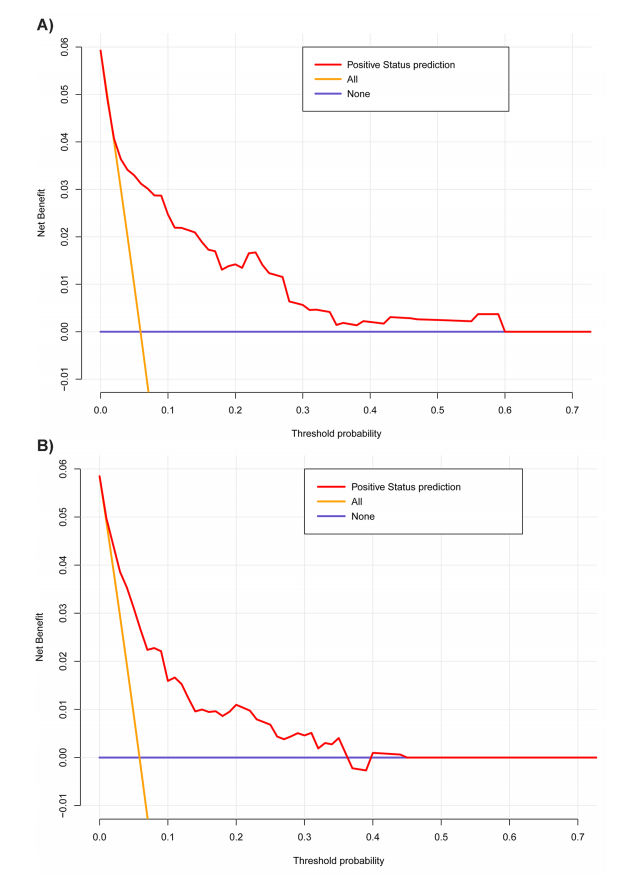
对训练集(A)和验证集(B)的nomogram进行决策曲线分析(Decision curve analysis, DCA)。DCA表明,在2-60%的阈值概率区间内,训练模型的净效益更高,在1-37%的阈值概率区间内,验证模型的净效益更高
结果:共纳入1152例患者,其中810例用于训练组,342例用于验证组。LWI的发生率为5.93%。多因素分析显示,年龄62岁及以上(奇比(or)=2.37, 95%可信区间(CI) 1.07-5.24)、Charlson合病指数3及以上(or =3.64, 95% CI 1.09-12.14)、Association Research Circulation osseiv期(or =2.16, 95% CI 1.03-4.54)、股骨偏位减小(or =2.41, 95% CI 1.16-5.03)和较高的控制营养状况评分(or =1.14, 95% CI 1.01-1.30)是LWI的独立危险因素。训练集的方差图一致性指数为0.773,Brier评分为0.049,内部验证后校正值为0.747和0.051。受试者工作特征曲线、校准曲线、Hosmer-Lemeshow检验和决策曲线分析在训练组和验证组均表现良好。
结论:本研究报道了5.93%的LWI发生率,并建立了ONFH THA患者LWI的风险预测模型,支持有针对性的筛查和干预,以协助外科医生评估行走能力和康复管理。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















不错,学习了。
54
学习了,谢谢分享
62
认真学习了
54
好文章,值得一读。
49
#股骨头坏死# #全髋关节置换术#
60