“手术刀征”,大家见过吗?
2023-05-07 李永超Li Spine脊柱 发表于上海
脊柱矢状位MRI T2WI脊髓局部性扭曲并向前移位,扩大的背侧脑脊液间隙形似手术刀,称为“手术刀征”。
先看一个病例:
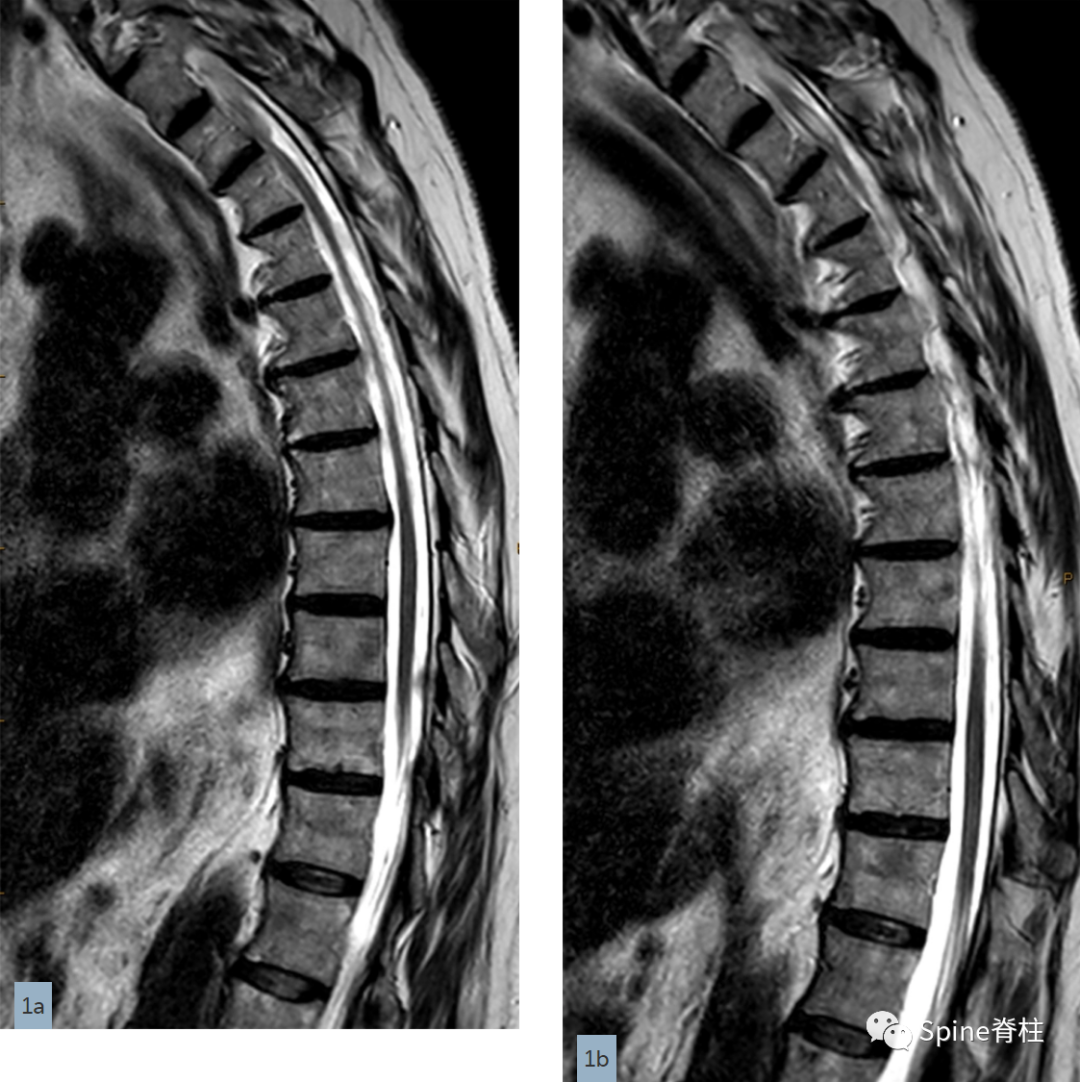
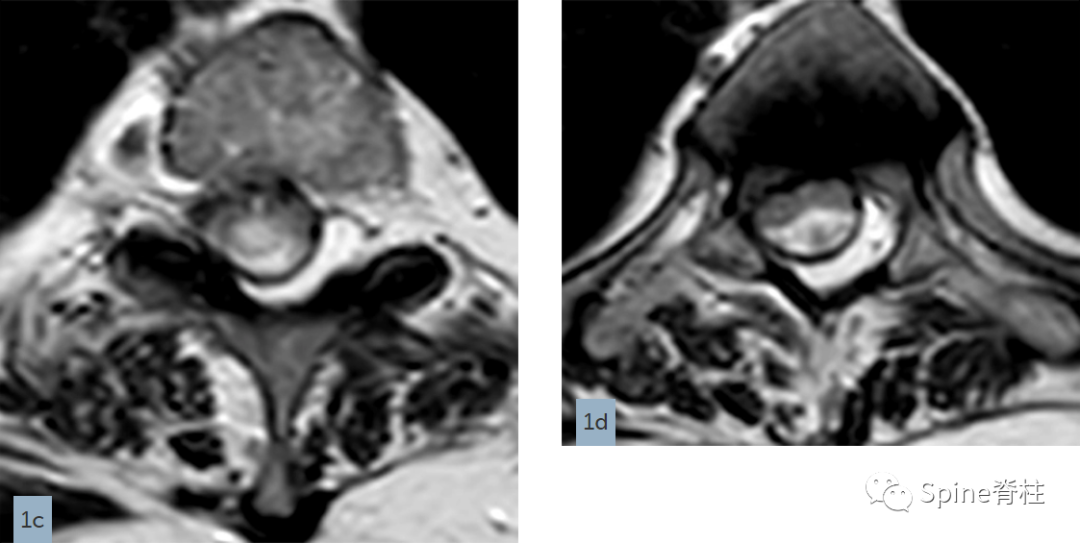
一名76岁的女性出现颈部和左臂疼痛。提供了矢状T2加权(1a和1b)和轴向T2加权图像(1c和1d)。结果是什么?你的诊断是什么?
影像发现:

影像诊断
T2-3背侧蛛网膜网带(dorsal arachnoid web,DAW)和脊髓空洞
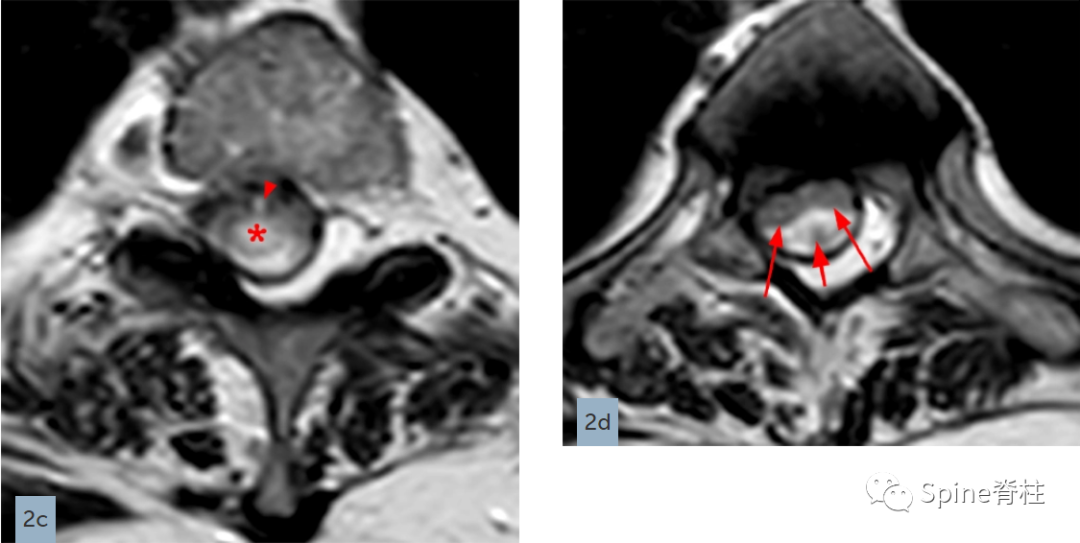
背侧蛛网膜网带是一种位于髓外硬膜下的增厚的横行束带状(bands)或网状(webs)蛛网膜组织,压迫脊髓背表面,导致慢性脊髓压迫和畸形。带状物和网状物在形态上彼此不同,但引起的问题类似,都是引起脊髓的损害。一般来说,带是一个简单的加厚带状结构,而网是一个更复杂的网络样网带。
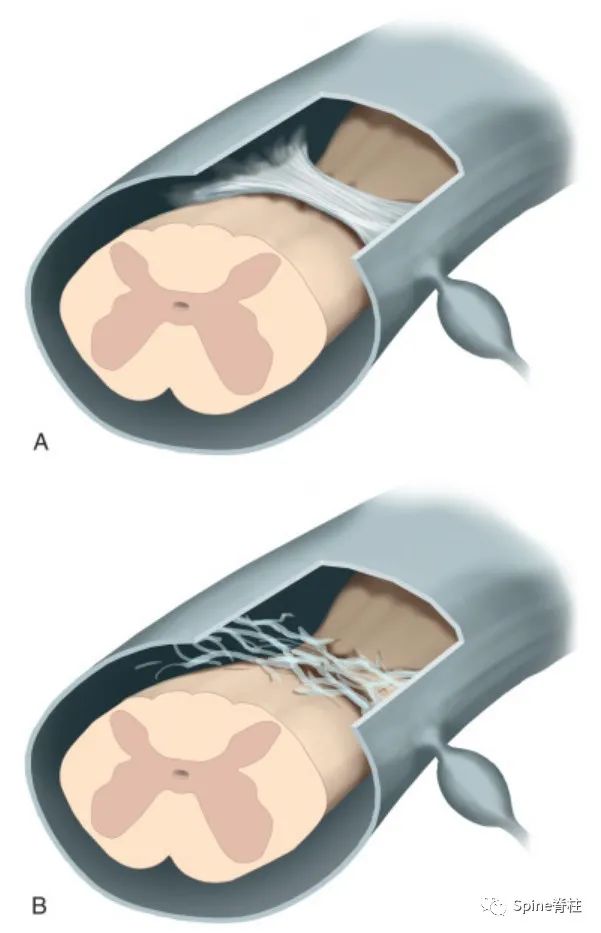
A为背侧蛛网膜束带,B为背侧蛛网膜网带
DAW多发生在中上段胸髓,因背侧蛛网膜网带的牵拉,可造成脊髓背侧局部受压凹陷、向前移位和背侧脑脊液间隙增宽,在MRI上呈现为一种特征性的影像表现,即“手术刀征”(scalpel sign)。同时,也常伴有脊髓受压平面上方的脊髓空洞。

对于不伴有脊髓空洞的DAW,MRI阅片时候要特别注意,不要漏诊。黄箭头处为该病典型的"手术刀征"
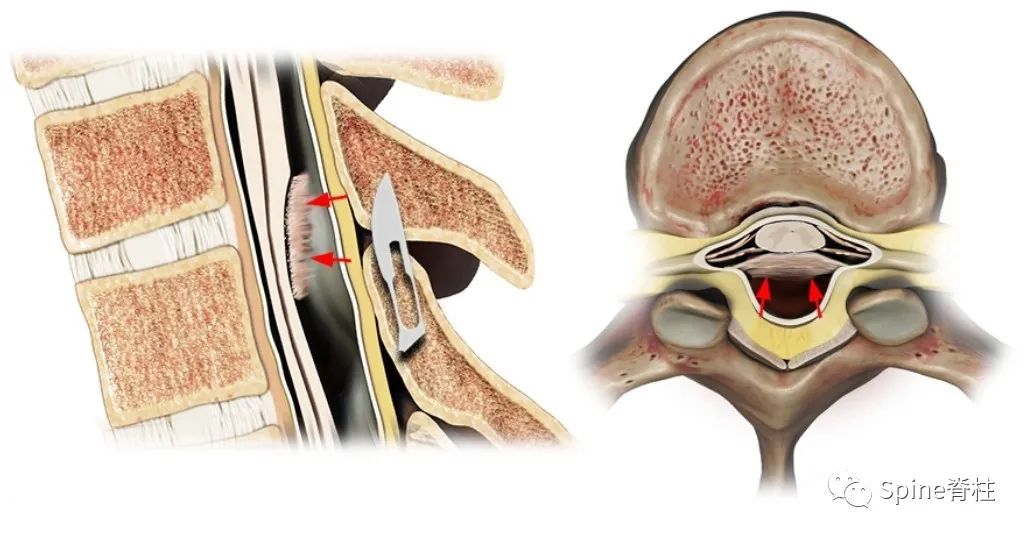

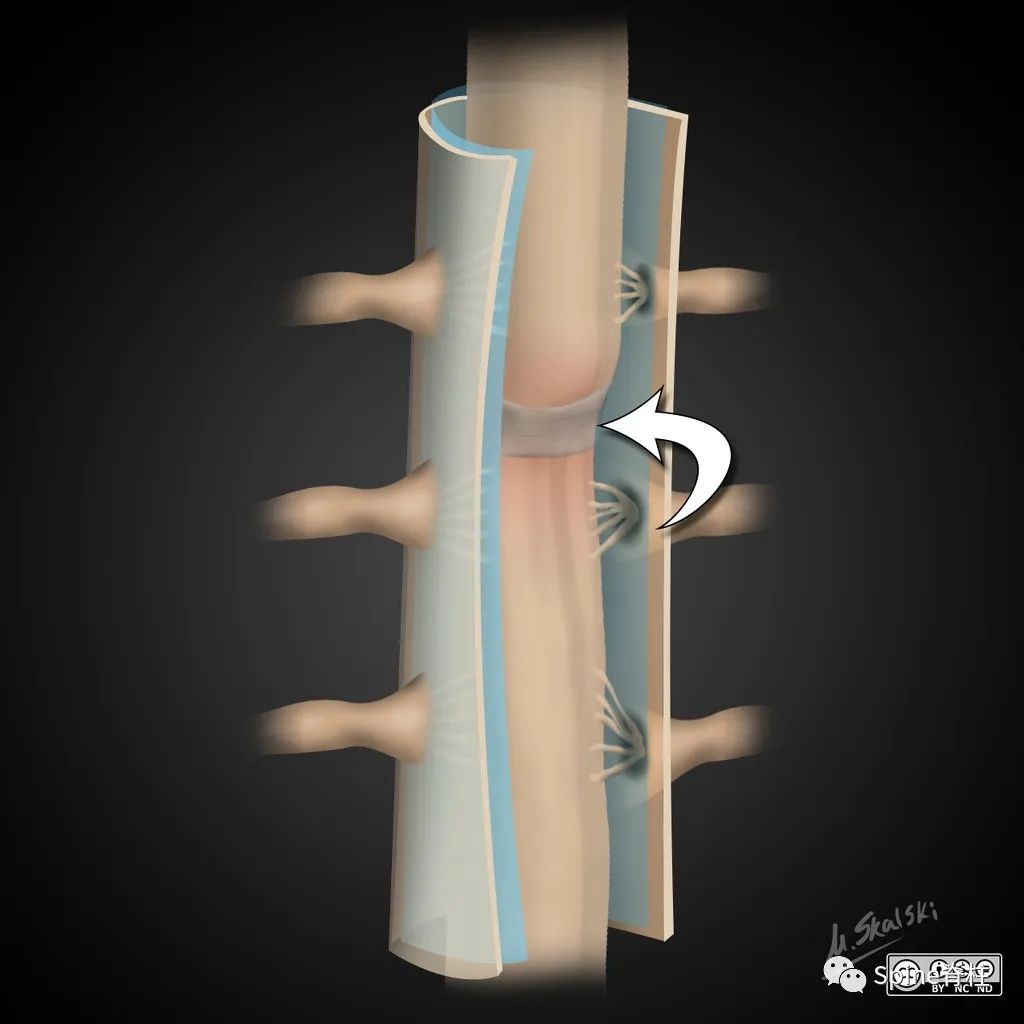
DAW需与腹侧脊髓疝 (ventral cord herniation)鉴别。矢状和轴向视图显示腹侧脑脊液丢失,部分脊髓通过小硬脑膜缺损(箭头)疝出。脊髓腹侧移位导致背侧蛛网膜下腔扩大,矢状面上出现“C”形背侧脊髓轮廓


腹侧脊髓疝
在国内,脊髓背侧蛛网膜网带主要是神经外科处理,及时发现,及时手术切除束带或网状带和脊髓空洞分流术,能挽回脊髓功能或阻止脊髓功能的恶化。大部分DAW病人及时手术治疗,预后较好。然而,这类病人有时因脊髓损害症状会就诊于骨科、脊柱外科和神经内科等科室,如不认识则可能会延误诊断与治疗,尤其是不伴有脊髓空洞的患者。
因此,应认识DAW特征性的影像表现“手术刀”征,及时请神经外科医生会诊或给患者指明诊治方向。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习打卡
106
学习
75
不错,学习了。
94
不错,学习了。
115