Blood:导致遗传性血小板减少症的PTPRJ功能性突变
2019-01-22 MedSci MedSci原创
遗传性血小板减少症(ITs)是一种以低血小板计数为特征的异质性疾病,可导致出血倾向。尽管对其遗传因素的研究获得了一定进展,但近50%的家族性血小板减少症患者的病因仍不明确。现Caterina Marconi等人对两对常染色体隐形血小板减少症的兄弟姐妹进行外显子测序,在PTPRJ基因上鉴定出两个等位基因功能丧失性突变。该基因编码受体样蛋白酪氨酸磷酸酶——PTPRJ(或CD148),在血小板和巨核细胞
遗传性血小板减少症(ITs)是一种以低血小板计数为特征的异质性疾病,可导致出血倾向。尽管对其遗传因素的研究获得了一定进展,但近50%的家族性血小板减少症患者的病因仍不明确。
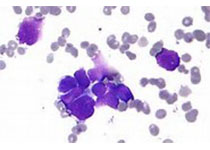
现Caterina Marconi等人对两对常染色体隐形血小板减少症的兄弟姐妹进行外显子测序,在PTPRJ基因上鉴定出两个等位基因功能丧失性突变。该基因编码受体样蛋白酪氨酸磷酸酶——PTPRJ(或CD148),在血小板和巨核细胞中大量表达。与预测效应一致,两个先证者的PTPRJ mRNA和蛋白都几乎完全缺失。
为进一步研究PTPRJ缺陷在体内造血作用中的致病作用,研究人员采用CRISPR/Case9敲除斑马鱼的ptprja(人PTPTJ的同源基因),导致活体CD41+血小板的数量显著降低。而且,在体外,患者的巨核细胞的成熟和先证者的SDF1驱动的迁移、血小板前体形成均受损。沉默人巨核细胞系的PTPRJ可再现在患者巨核细胞中所观察到的功能缺陷。
该基因由PTPRJ突变引起,表现为一种非综合征性的血小板减少症,特征为自发性出血、小血小板、血小板对GPVI激动剂胶原和convulxin的反应受损。上述血小板功能缺陷可归因于Src家族激酶的活化减少。
综上所述,本研究揭示了一种新的IT形成形式以及PTPRJ在血小板生成中的基本作用。
原始出处:
Caterina Marconi, et al. A new form of inherited thrombocytopenia caused by loss-of-function mutations in PTPRJ. Blood 2018 :blood-2018-07-859496; doi: https://doi.org/10.1182/blood-2018-07-859496
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PTPRJ#
72 举报
#遗传性#
69 举报
#功能性#
75 举报
#血小板减少#
81 举报
好
96 举报
好好好好好好好好
119 举报