GUT:武汉协和医院团队报导非侵入性磁控取样胶囊内窥镜技术
2021-10-10 haibei MedSci原创
与手术相比,MSCE可以精确地获得有关肠道菌群和代谢物的数据,这些数据在不同的肠道区域和疾病模型中被有效区分。
肠道菌群和消化道的代谢物可以提供生物信息,这与个人的健康状况有关。有趣的是,从不同阶段的结直肠肿瘤患者获得的粪便样本可以提供粪便微生物不同阶段表型的证据。经过近十年的研究,来自25个不同机构的专家共同证明了人类肠道微生物组中存在肠型。 肠道微生物群失调已被证明不仅影响消化系统疾病的进程,也影响心血管和代谢疾病以及癌症。因此,肠道菌群分析被认为在众多人类疾病的筛选、诊断、严重程度评估、治疗方案选择和预后评估中非常有用。
同时,代谢物是各种疾病的潜在生物标志物,例如,油酸,一种脂肪酸,可以减少肠道炎症,降低结肠直肠癌发展的可能性。此外,亚油酸在非酒精性脂肪肝(NAFLD)患者中的积累可以导致非酒精性脂肪肝相关肝细胞癌的进展。还有一项临床研究表明,五种代谢物的特征与肾脏疾病的临床标志物密切相关。值得注意的是,代谢物也可用于预测治疗反应,比如有四种代谢物在抗性高血压中增加。
目前,消化道样本采集主要有三种方法,即呼气式氢气检测、粪便微生物检查和无创内窥镜检查。然而,这些方法的主要缺点包括:规格低;呼气式检测不能详细反映微生物群,粪便样本检查不能揭示真实状态下特定肠道区域的生物信息;内窥镜检查的创伤性、不便和费力的消化道准备要求。
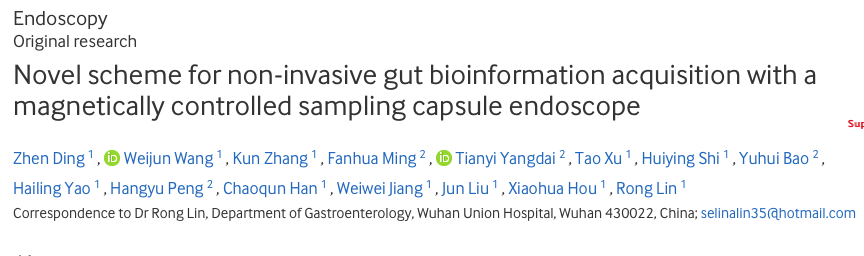
最近,武汉协和医院的研究人员进行了一项探究,旨在开发一种精确的磁控取样胶囊内窥镜(MSCE),以方便、无创和准确地获取消化道生物信息,用于疾病诊断和评估。
该研究包括了对照组和抗生素引起的腹泻组,MSCE和手术都用于对受试者空肠和回肠消化道内容物进行采样,然后研究人员将消化道内容物用于微生物组分析和代谢组学分析。
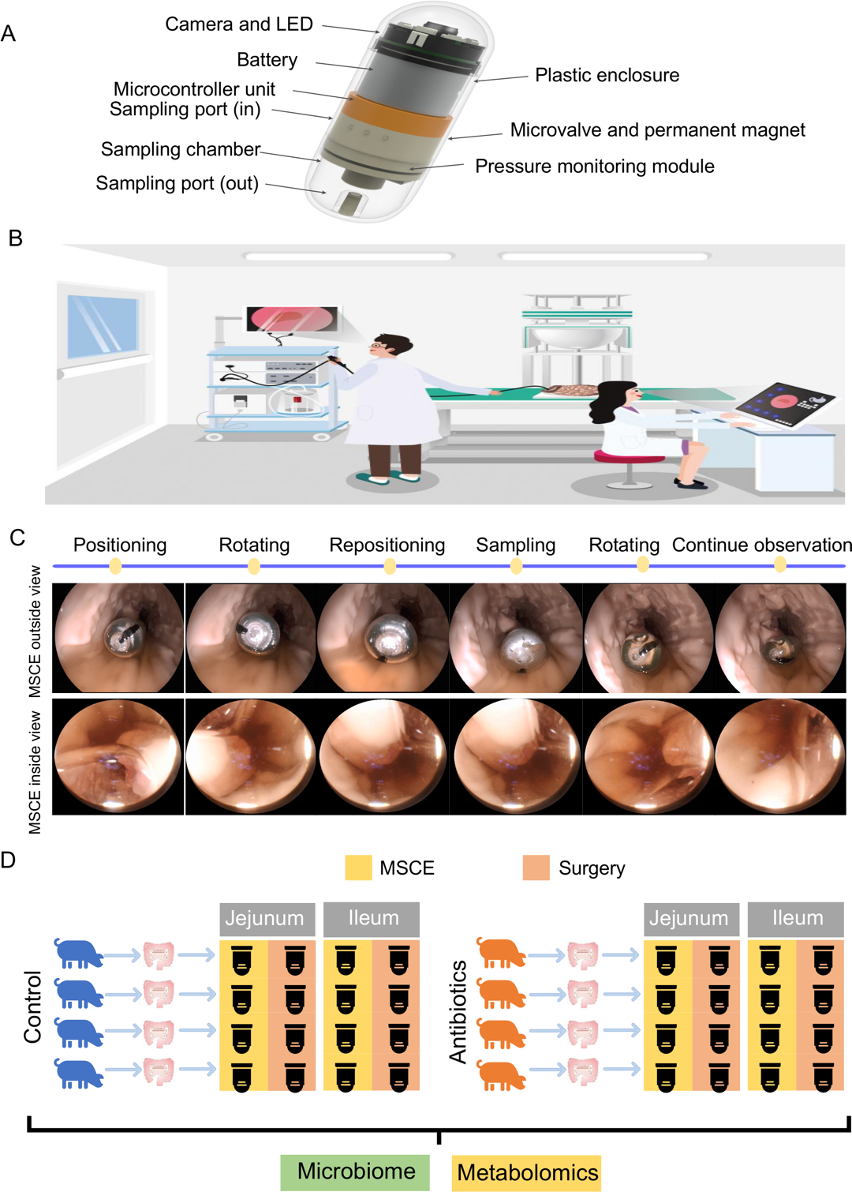
磁控采样胶囊内窥镜(MSCE)能够对肠道内容进行采样。
结果显示,与手术相比,MSCE可以精确地获得有关肠道菌群和代谢物的数据,这些数据在不同的肠道区域和疾病模型中被有效区分。利用MSCE,研究人员检测到在抗生素诱导的腹泻模型中,类杆菌、盖茨菌和放线菌的丰度和海马酸水平急剧下降,以及志贺埃希氏菌的丰度和2-吡咯烷酮水平增加。
此外,MSCE介导的采样发现了特定的肠道微生物群/代谢物,包括肠球菌、Lachnospiraceae、乙酰-L-肉碱和琥珀酸,它们与代谢性疾病、癌症和神经系统疾病有关。并且,MSCE表现出良好的密封特性,采样后没有污染。
因此, 该研究提出了一种新开发的MSCE,它可以在磁控制下通过直接可视化的手段,无创和准确地获取肠道生物信息,这可能进一步帮助疾病的预防、诊断、预后和治疗。
原始出处:
Zhen Ding et al. Novel scheme for non-invasive gut bioinformation acquisition with a magnetically controlled sampling capsule endoscope. GUT (2021).

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#侵入性#
127 举报
#非侵入性#
104 举报
学习的
129 举报
学习
139 举报
#协和#
106 举报
#协和医院#
119 举报
#内窥镜#
95 举报