JECCR :复旦大学董玲/张思研究团队阐述肠道微生物介导的肿瘤免疫调控机制
2021-07-05 JACKZHAO MedSci原创
综述文章:阐述了肠道微生物介导的肿瘤免疫调控机制。

Liu, X., Chen, Y., Zhang, S. et al. Gut microbiota-mediated immunomodulation in tumor. J Exp Clin Cancer Res 40, 221 (2021). https://doi.org/10.1186/s13046-021-01983-x
近日,复旦大学附属中山医院董玲主任医师与复旦大学基础医学院张思教授联合在Springer Nature出版集团出版的肿瘤领域权威期刊Journal of Experimental & Clinical Cancer Research,JECCR(影响因子=11.16)在线发表题为Gut microbiota-mediated immunomodulation in tumor的综述文章,阐述了肠道微生物介导的肿瘤免疫调控机制。
人体肠道内定植着数以亿计的微生物,构成肠道菌群。肠道菌群在许多生理病理过程中发挥重要作用。近几年的研究发现肠道菌群也参与肿瘤的发生发展,并影响个体对治疗的敏感性,但潜在的机制仍有待探寻。文章聚焦于肠道菌群对肿瘤免疫的影响,从固有免疫和适应性免疫两个角度进行论述,并总结了肠道菌群参与肿瘤免疫调节的可能机制,即PAMP-TLR信号通路、肠菌的代谢产物、调节次级淋巴器官的免疫微环境。
最后,文章列举了既往文献报道的肠道菌群和免疫检查点抑制剂(ICI)疗效的关联,并讨论了通过调节肠道菌群改善ICI疗效的可行性。尽管大量动物实验和临床研究提示肠道菌群可以影响肿瘤免疫并作为肿瘤免疫治疗的靶点,但其中仍有许多未知数,且现有研究结果间一致性较差。加之临床情况的复杂性,肠道菌群能否应用于临床实践尚值得商榷,这也是未来研究努力的方向。

肿瘤免疫监视可以分成两个部分,即固有免疫和适应性免疫。前者包括各种髓系细胞和先天淋巴样细胞,如自然杀伤(NK)细胞和巨噬细胞。NK细胞可通过抗体依赖的细胞介导的细胞毒作用(ADCC)、FAS-FASL途径、穿孔素-颗粒酶B等途径杀伤肿瘤细胞。除了ADCC和调理作用,巨噬细胞还能作为抗原提呈细胞发挥抗肿瘤效应。适应性免疫起始于T细胞受体(TCR)识别肿瘤抗原,树突状细胞(DC)在其中发挥重要作用。
肿瘤形成过程中产生的新抗原被释放出来并被DC捕获、加工,继而以抗原肽-MHC复合物(pMHC)的形式呈递给T细胞。TCR和pMHC相互作用,加之共刺激信号,最终激活了效应T细胞。激活的T细胞可以特异性靶向肿瘤细胞,通过直接的细胞毒作用杀伤肿瘤细胞或产生细胞因子以招募更多免疫细胞。

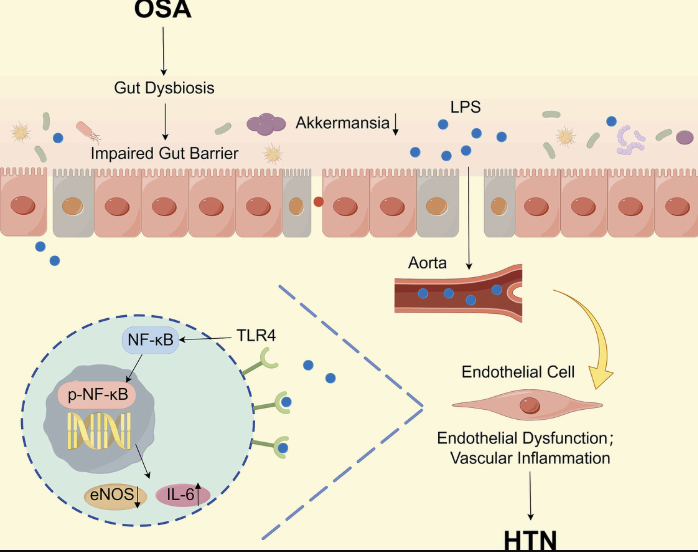
肠道菌群既可以局部也可以系统性地影响肿瘤免疫。在肿瘤局部,梭菌属可通过TLR4/MYD88信号通路作用于结肠癌细胞。NF-κB的激活促进了炎症因子如TNF-α、IL-6的的转录,继而引起抑制性的髓样细胞在肿瘤微环境中聚集。就全身而言,细菌鞭毛和TLR5的相互作用引起循环中IL-6的水平升高,继而招募更多γδT细胞产生免疫抑制的半乳糖凝集素-1,最终加速了远处肿瘤的进展。不仅如此,肠肝循环使肠道菌群来源的病原相关分子模式(PAMP)和代谢产物能参与肝癌的发生发展。
一方面,肝癌时由于菌群紊乱和肠黏膜屏障通透性增加,门静脉和循环中脂多糖(LPS)的水平显著提高,继而激活肝星状细胞的NF-κB,诱导炎性细胞因子的产生。这些细胞因子促进巨噬细胞和髓源性抑制细胞(MDSC)迁移到肝脏。同样的,源于肠道的LTA通过诱导COX2表达促进PGE2的产生,后者作用于免疫细胞上的PTGER4受体以抑制抗肿瘤免疫,表现为IFN-γ和TNF-α分泌减少,CD103+DC减少,调节性T细胞(Treg)增多。
另一方面,抗生素杀灭了参与胆汁酸转化的G+菌,从而增加了CXCL16的表达。上调CXCL16诱导CXCR6+NKT细胞聚集并激活,最终抑制肝癌生长。除了上述机制,肠道菌群还能通过细菌易位调节次级淋巴器官的免疫微环境。比如,环磷酰胺介导的脾脏pTh17细胞聚集依赖于部分G+菌易位到脾脏,细菌易位增加了循环CD8+T细胞,并提高了瘤内CTL/Treg的比值。
该文章的第一作者为复旦大学刘心怡博士,通讯作者为中山医院董玲主任医师及复旦大学基础医学院张思教授。
参考资料:
Liu, X., Chen, Y., Zhang, S. et al. Gut microbiota-mediated immunomodulation in tumor. J Exp Clin Cancer Res 40, 221 (2021). https://doi.org/10.1186/s13046-021-01983-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ECC#
84
厉害
102
#微生物#
85
厉害
117
#调控机制#
114
#复旦#
78
#研究团队#
105
#免疫调控#
80
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
91